Arch Iran Med. 27(7):400-402.
doi: 10.34172/aim.28804
Case Report
Neuromyelitis in a Patient with Rheumatoid Arthritis: A Case Report
Fuyong Qiang Conceptualization, Investigation, Methodology, Resources, Writing – original draft, 1, # 
Zhi Li Data curation, Validation, Writing – original draft, 1, # 
Lanfang Chen Formal analysis, Resources, Visualization, 1
Dan Xuan Validation, Writing – review & editing, 1
Jun Sheng Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing, 1, * 
Author information:
1Department of Rheumatism and Immunology, The First Affiliated Hospital of Wannan Medical College, Wuhu, Anhui, China
#Contributed equally to the work as first authors.
Abstract
A patient with longstanding rheumatoid arthritis (RA) complained of spinal cord symptoms after RA relapse. Contrast MRI demonstrated neuromyelitis in the upper thoracic spinal cord, and anti-aquaporin-4 (anti-AQP4) antibody was positive in the serum and cerebrospinal fluid (CSF). Neuromyelitis optica spectrum disorder (NMOSD) was diagnosed after excluding central nervous system (CNS) infection and tumor, and spinal cord symptoms were relieved after high dose of glucocorticoid and immunosuppressant were initiated for treatment.
Keywords: Aquaporin-4, Neuromyelitis, Rheumatoid arthritis
Copyright and License Information
© 2024 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Qiang F, Li Z, Chen L, Xuan D, Sheng J. Neuromyelitis in a patient with rheumatoid arthritis – a case report. Arch Iran Med. 2024;27(7):400-402. doi: 10.34172/aim.28804
Introduction
Rheumatoid arthritis (RA) is a systemic autoimmune disease that mainly involves peripheral joints. Nerve damage occurs in about 20% of patients. The peripheral sensory and motor nerves are commonly involved, and the most common symptoms are limb weakness and sensory abnormalities due to vascular ischemia, axonal degeneration, and neuronal demyelination, which are caused by vasculitis.1 Central nervous system (CNS) involvements in RA patients includes meningitis, optical atrophy, and cerebral vasculitis.2,3 In addition, cervical myelopathy caused by cervical spine cord compression is the most common among these alterations in patients with longstanding RA.4 However, neuromyelitis in RA is rare. Here, we present a case of RA with neuromyelitis.
Case Report
A 61-year-old female complained of swelling and pain in the proximal interphalangeal joints and metacarpophalangeal of both hands accompanied by morning stiffness > 1 hour per day for ten years. She was diagnosed as RA as both rheumatoid factor (RF) and anti-cyclic citrullinated protein (anti-CCP) antibody were positive. The patient refused to take methotrexate, and low-dose prednisone combined with leflunomide and sulfasalazine were prescribed for treatment. The joint symptoms were relieved after three years of treatment and the patient stopped taking all drugs spontaneously. Swelling and pain of metacarpophalangeal joints, wrist joints, and ankle joints re-occurred one year later accompanied by acupuncture pain, pruritus and persistent superficial hypoesthesia on the back of bilateral nipple plane. No skin lesions were observed in this area and the patient did not exhibit any systemic signs such as high fever, weight loss, heart failure, or gastrointestinal bleeding. Laboratory investigations revealed erythrocyte sedimentation rate (ESR) of 94 mm/h, C-reactive protein (CRP) of 47.5 mg/L, and IgG of 23.73 g/L. IgM-RF and anti-CCP antibody were at 86.5 IU/mL (normal < 20) and 386.0 U/mL (normal < 25), respectively. Complete blood count and tests for liver function, renal function, tumor markers, urinalysis, cardiac enzymes, complement, PPD-test and T-spot were all normal. Tests for hepatitis, syphilis, HIV, and autoantibody profile were all negative. Schirmer’s test and Saxon test showed scores of 12 mm/5 min and 3.5 g/2 min, respectively. The patient refused to undergo sialography, and salivary gland ultrasonography was performed which indicated mild atrophy of bilateral parotid glands. Lip biopsy revealed no significant lymphocyte infiltration. No abnormal changes were observed in brain MRI or MRA (Figure 1E-H). MRI showed longitudinally extensive T1-weighted and T2-weighted hyperintensity in the upper thoracic spinal cord (T1-T4) and contrast MRI T2-weighted demonstrated enhanced high signal change (Figure 1A-C). Biochemical, routine and microbial tests of cerebrospinal fluid (CSF) were negative. Immunoglobulin levels were normal in the CSF: IgA 4 mg/L (normal range 0-6 mg/L), IgG 25 mg/L (normal range 10-40 mg/L), IgM 7.4 mg/L (normal range 0-13 mg/L). In addition, the CSF was negative for oligoclonal IgG bands. Anti-aquaporin-4 (AQP4) antibody was positive and anti-myelin oligodendrocyte glycoprotein antibody was negative in the serum and CSF. The patient was diagnosed as RA complicated by neuromyelitis optica spectrum disorder (NMOSD); her expanded disability status scale (EDSS)5 was 2.0. She was treated with 1000mg intravenous methylprednisolone for 3 days and 500mg intravenous methylprednisolone for 3 days. Maintenance treatment included a tapering high dose of oral prednisolone. In addition, intravenous cyclophosphamide 1g once a month for half a year was initiated then altered to oral azathioprine for maintenance treatment. Acupuncture pain, pruritus, and superficial hypoesthesia were relieved after treatment. Thoracic spinal cord MRI demonstrated that myelitis was significantly improved one year later (Figure 1D).
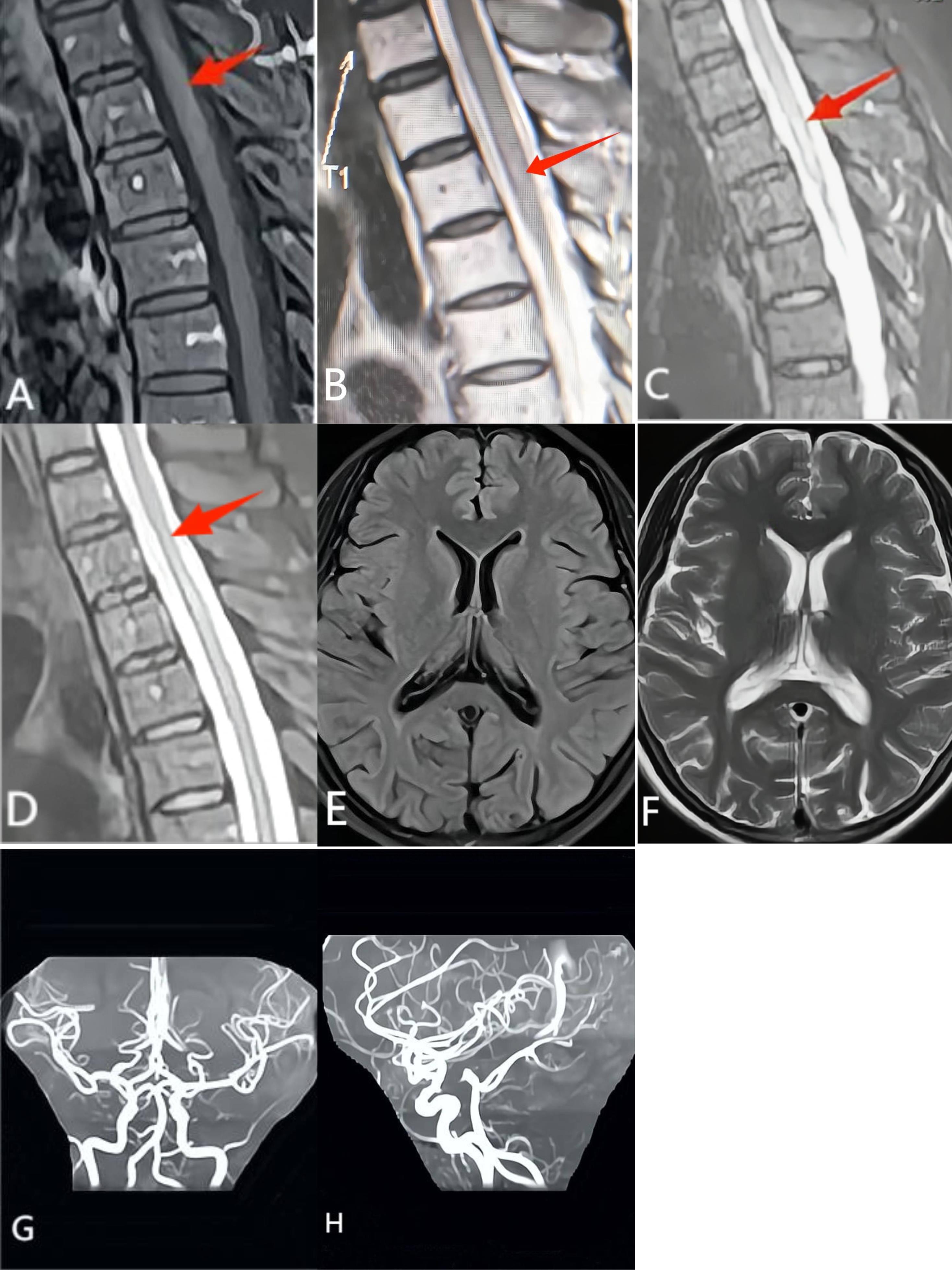
Figure 1.
Magnetic Resonance Image (MRI) of the Upper Thoracic Spinal Cord in the Patient. (A-B) MRI shows longitudinally extensive T1-weighted and T2-weighted hyperintensity in the upper thoracic spinal cord (T1-T4) (red arrow). (C) Contrast MRI T2-weighted demonstrates enhanced high signal change (red arrow). (D) High signal change was significantly improved after treatment one year later (red arrow). (E-H) No abnormal changes were observed in either brain MRI or MRA
.
Magnetic Resonance Image (MRI) of the Upper Thoracic Spinal Cord in the Patient. (A-B) MRI shows longitudinally extensive T1-weighted and T2-weighted hyperintensity in the upper thoracic spinal cord (T1-T4) (red arrow). (C) Contrast MRI T2-weighted demonstrates enhanced high signal change (red arrow). (D) High signal change was significantly improved after treatment one year later (red arrow). (E-H) No abnormal changes were observed in either brain MRI or MRA
Discussion
In the present case, the patient had typical joint symptoms as well as positive RF and anti-CCP antibody, which conformed to the 2010 diagnostic criteria for RA established by the American Academy of Rheumatology/European Alliance Against Rheumatism (ACR/EULAR).6 The joint symptoms were relieved after treatment. However, the patient demonstrated involvement of the spinal cord besides joint symptoms when RA re-occurred. Contrast MRI indicated neuromyelitis in the upper thoracic spinal cord and anti-AQP4 antibody was positive in the serum and CSF. No evidence of infection or tumor was found in the CNS. Therefore, the patient conformed to the 2015 diagnostic criteria for NMOSD.7 Systemic lupus erythematosus (SLE) and Sjogren’s syndrome (SS) are the most common reasons in connective tissue disease-associated neuromyelitis as these diseases can lead to spinal cord vasculitis by forming many immune complexes.8 However, SLE and SS could be excluded in this case as a result of negative autoantibody profile, normal hemogram, negative urine analysis, negative Schirmer’s test and Saxon test as well as negative lip biopsy. Visual impairment was reported as the prominent manifestation in some previous reports.9,10 However, spinal cord involvement was the main manifestation in this case. Anti-AQP4 antibody is closely associated with occurrence of NMOSD,11 the proportion of positive anti-AQP4 antibody and the titer of anti-AQP4 antibody were all increased in NMOSD, but this antibody was not detected in SLE and RA patients in a previous study.12 Regarding the genetic background, the HLA-DRB1 *04 allele increases susceptibility to seropositive RA and NMOSD,13,14 and we speculate that a common genetic locus leads to the simultaneous occurrence of both diseases.
We reported a rare case of RA complicated with NMOSD. However, we could not conclude whether RA and NMO were two isolated disorders or NMO was caused by the RA relapse. The relationship between RA and NMO needs further studies for clarification.
Competing Interests
The authors declare that they have no conflict of interest.
Ethical Approval
This article has received ethical approval from Ethics Committee of Wannan Medical College.
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
References
- Maiuolo J, Muscoli C, Gliozzi M, Musolino V, Carresi C, Paone S. Endothelial dysfunction and extra-articular neurological manifestations in rheumatoid arthritis. Biomolecules 2021; 11(1):81. doi: 10.3390/biom11010081 [Crossref] [ Google Scholar]
- McKenna MC, Vaughan D, Bermingham N, Cronin S. Rheumatoid arthritis presenting as rheumatoid meningitis. BMJ Case Rep 2019; 12(1):bcr-2018. doi: 10.1136/bcr-2018-226649 [Crossref] [ Google Scholar]
- Ohno T, Matsuda I, Furukawa H, Kanoh T. Recovery from rheumatoid cerebral vasculitis by low-dose methotrexate. Intern Med 1994; 33(10):615-20. doi: 10.2169/internalmedicine.33.615 [Crossref] [ Google Scholar]
- Janssen I, Nouri A, Tessitore E, Meyer B. Cervical myelopathy in patients suffering from rheumatoid arthritis-a case series of 9 patients and a review of the literature. J Clin Med 2020; 9(3):811. doi: 10.3390/jcm9030811 [Crossref] [ Google Scholar]
- Piri Çinar B, Güven Yorgun Y. What we learned from the history of multiple sclerosis measurement: expanded disability status scale. Noro Psikiyatr Ars 2018; 55(Suppl 1):S69-75. doi: 10.29399/npa.23343 [Crossref] [ Google Scholar]
- Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 2010; 62(9):2569-81. doi: 10.1002/art.27584 [Crossref] [ Google Scholar]
- Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 2015; 85(2):177-89. doi: 10.1212/wnl.0000000000001729 [Crossref] [ Google Scholar]
- Kolfenbach JR, Horner BJ, Ferucci ED, West SG. Neuromyelitis optica spectrum disorder in patients with connective tissue disease and myelitis. Arthritis Care Res (Hoboken) 2011; 63(8):1203-8. doi: 10.1002/acr.20486 [Crossref] [ Google Scholar]
- Wang JC, Tow S, Aung T, Lim SA, Cullen JF. The presentation, aetiology, management and outcome of optic neuritis in an Asian population. Clin Exp Ophthalmol 2001; 29(5):312-5. doi: 10.1046/j.1442-9071.2001.00442.x [Crossref] [ Google Scholar]
- Wang CR, Hsu SM, Chen YC. Rheumatoid arthritis with aquaporin-4 antibody-positive neuromyelitis optica receiving rituximab therapy. Arch Rheumatol 2022; 37(1):153-5. doi: 10.46497/ArchRheumatol.2022.8688 [Crossref] [ Google Scholar]
- Papadopoulos MC, Verkman AS. Aquaporin 4 and neuromyelitis optica. Lancet Neurol 2012; 11(6):535-44. doi: 10.1016/s1474-4422(12)70133-3 [Crossref] [ Google Scholar]
- Stathopoulos P, Chastre A, Waters P, Irani S, Fichtner ML, Benotti ES. Autoantibodies against neurologic antigens in nonneurologic autoimmunity. J Immunol 2019; 202(8):2210-9. doi: 10.4049/jimmunol.1801295 [Crossref] [ Google Scholar]
- Padyukov L. Genetics of rheumatoid arthritis. Semin Immunopathol 2022; 44(1):47-62. doi: 10.1007/s00281-022-00912-0 [Crossref] [ Google Scholar]
- Ghafouri-Fard S, Azimi T, Taheri M. A comprehensive review on the role of genetic factors in neuromyelitis optica spectrum disorder. Front Immunol 2021; 12:737673. doi: 10.3389/fimmu.2021.737673 [Crossref] [ Google Scholar]