Arch Iran Med. 27(10):588-594.
doi: 10.34172/aim.31230
Systematic Review
Epidemiology of Post-traumatic Stress Disorder in Iranian Population From 2019 to 2024: A Systematic Review and Meta-analysis
Asad Imani Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing, 1 
Shahram Molavynejad Conceptualization, Supervision, Writing – review & editing, 2, * 
Mojgan Khademi Supervision, 3
Mohammad Adineh Conceptualization, 2
Elham Shafiei Formal analysis, Methodology, 4
Mohsen Savaie Conceptualization, Writing – review & editing, 5
Author information:
1Student Research Committee, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2Nursing Care Research Center in Chronic Diseases, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
3Social Determinants of Health Research Center, School of Nursing and Midwifery, Lorestan University of Medical Sciences, Khorramabad, Iran
4Psychosocial Injuries Research Center, Ilam University of Medical Sciences, Ilam, Iran
5Pain Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Abstract
Background:
Post-traumatic stress disorder (PTSD) is a disorder that arises from experiencing traumatic events such as traffic accidents, war, natural disorders, and job incidents. This study focused on determining the epidemiology of PTSD in the Iranian population from 2019 to 2024.
Methods:
In this systematic review and meta-analysis, we explored databases such as PubMed, Embase, Web of Knowledge, Scopus, and Magiran to achieve a maximum variety of screened articles. The quality of the included articles was evaluated using the STROBE checklist. For data analysis, due to the variation in reporting the PTSD prevalence across the reviewed articles, heterogeneity was assessed using the I2 index, and a random effect model was applied to account for this variation.
Results:
Out of 800 articles found in the initial review, only 15 articles were entered in the final analysis based on inclusion and exclusion criteria, with a total of 9868 participants. The overall PTSD prevalence in the Iranian population was 31.87% (95% confidence interval [CI]=17.87- 45.87, I2=95.29%, P<0.001). Additionally, PTSD prevalence in men (36.64%) was higher than in women (35.52%).
Conclusion:
The prevalence of PTSD in young Iranian men is relatively high, and there was no statistically significant decrease in PTSD prevalence between 2019 and 2024.
Keywords: Iran, Post-traumatic stress disorder, Prevalence, Trauma
Copyright and License Information
© 2024 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Imani A, Molavynejad S, Khademi M, Adineh M, Shafiei E, Savaie M. Epidemiology of post-traumatic stress disorder in Iranian population from 2019 to 2024: a systematic review and meta-analysis. Arch Iran Med. 2024;27(10):588-594. doi: 10.34172/aim.31230
Introduction
Trauma has been one of the leading causes of disability and death in recent decades.1 A study on the prevalence of trauma among 24 European countries found that 70.4% of people suffered one or more major trauma during the year.2 The prevalence of trauma in Iran has been reported in various studies, ranging between 61.70%3 to 89.2%,4 making it the second leading cause of death.5 Iran is prone to events such as earthquakes, wars, road traffic accidents, and floods.6 Given the relatively high incidence of trauma in Iran and the psychosocial responses such as post-traumatic stress disorder (PTSD), it seems that investigating this phenomenon in research studies should always be considered.7
PTSD is associated with work-related problems, lower quality of life, functional impairments, and physical health problems.8 Individuals with PTSD cases may face a prolonged recovery process, with about 10 % of individuals experiencing long-term psychological effects and chronic PTSD.9 A study in the United States revealed that the prevalence of PTSD one year after trauma ranged from 2.3% to 9.1%, with a lifetime prevalence from 3.4% to 26.9%.10 A study showed that the patterns of trauma in Iran and individual responses such as PTSD are constantly evolving.11 In Iran, different studies have investigated PTSD in relation to job-related trauma,12-16 accidents,3 wars,17 floods,18,19 the COVID-19,20-22 and childbirth.23,24 All these studies were conducted between 2019 and 2024.
Since the prevalence of stressful events varies across different periods, access to updated statistics in the form of a meta-analytic study will undoubtedly help to understand the true significance of the crisis. However, these epidemiological studies were conducted locally with limited sample sizes, making them insufficient for providing clear and useful information for high-level health decision-making. Health decision-makers cannot make decisions based on small and localized studies,25 nor can they generalize the prevalence of PTSD found in such studies to the entire Iranian society.26 Health authorities need to be aware of the actual prevalence of PTSD to develop an accurate crisis control map and effective operational plans. This is possible only through a national study or a meta-analysis of multiple studies. Therefore, a systematic review and meta-analysis of PTSD research can provide useful and concise information to health decision-makers for the management and prevention of this disorder. Thus, our primary objective was to conduct a study on the prevalence of PTSD in Iran from 2019 to 2024.
Materials and Methods
Search Strategies
Due to the broad scope of trauma-related topics and the variety of studies, we searched databases of PubMed, MEDLINE via OVID, Web of Knowledge, Wiley, Scopus, Magiran, SID, and Google Scholar with the keywords, including trauma, trauma in Iran, stress disorder, post-traumatic stress disorder, post-traumatic neuroses, and chronic post-traumatic stress disorder.
Moreover, to find articles related to the topic, we used combinations of Job and PTSD, Trauma and PTSD, War and PTSD, Earthquake and PTSD, Flood and PTSD. Other Boolean operators were used such as Trauma OR Event, Trauma OR Incident, Trauma Prevalence OR Trauma Incidence, PTSD NOT Anxiety, and PTSD NOT Stress. The searches in Google Scholar, Magiran, and SID were conducted only using the main keywords because they were not sensitive to the Boolean operators. However, searches in the other databases were carried out by combining words with Boolean operators.
Inclusion and Exclusion Criteria
Inclusion Criteria
-
All subjects exposed to traumatic events (incidents causing physical, emotional, spiritual, or psychological harm) such as wars, earthquakes, job-related stress, childbirth, and floods were included.
-
Articles carried out on Iranian populations.
-
Articles published in Persian or English.
-
Articles published between 2019 and 2024 (New statistics are always a better basis for health decision-makers. On the other hand, this period of time coincided with the COVID-19 pandemic, allowing us to investigate its effect on the prevalence of PTSD in Iran).
Exclusion Criteria
-
Full-text not available.
-
Articles published with qualitative approaches, case reports, letters to editors, and interventional studies (to maintain a quantitative approach and cohesiveness in the final analysis).
Qualification of Studies
The quality of studies was evaluated using the standard 22-item STROBE checklist. The checklist items are related to the issue and abstract (question 1), introduction (questions 2 and 3), methodology (questions 4-12), results (questions 13-17), discussion (questions 18-21), and information on funding (question 22).27 The questions mentioned in the pertinent section of the article were awarded one point if present, or zero if absent. According to consensus among the research team, articles that achieved 75% of the total score (16 points) were included in the meta-analysis.
Data Extraction
The abstracts and titles of the papers were independently reviewed by two independent reviewers according to the inclusion and exclusion criteria. Any cases of disagreement were resolved through discussion, and if necessary, all researchers reached a consensus to handle remarkable disagreements. Then, articles that met the inclusion criteria were categorized by study characteristics, including author, study location, year of publication, study method, events, overall PTSD prevalence, age range, PTSD prevalence by gender, and study population.
Statistical Analysis
The main objective of this study was to determine the prevalence of overall PTSD, as well as prevalence in men and women. Although examining heterogeneity in prevalence studies is not mandatory, it was investigated in the present study due to the variation in reported prevalence levels across the reviewed studies. The I2 index was employed to assess the heterogeneity of the studies, with values of < 25%, 25-75%, and > 75% representing low, moderate, and high heterogeneity, respectively.
One of the most effective approaches to deal with statistical heterogeneity in studies is to investigate the underlying causes by performing metaregression. In this study, metaregression analysis was conducted using STATA (v.17) to examine the relationship between PTSD prevalence and the year of study, study location, and event type.
Results
In the initial search, 800 articles were identified, and after reviewing their titles, only 300 were considered for screening. Among these, 250 articles failed to meet the inclusion criteria for further review. Eventually, 15 articles were included for meta-analysis and systematic review despite their full texts were accessible and contained sufficient information (Figure 1).
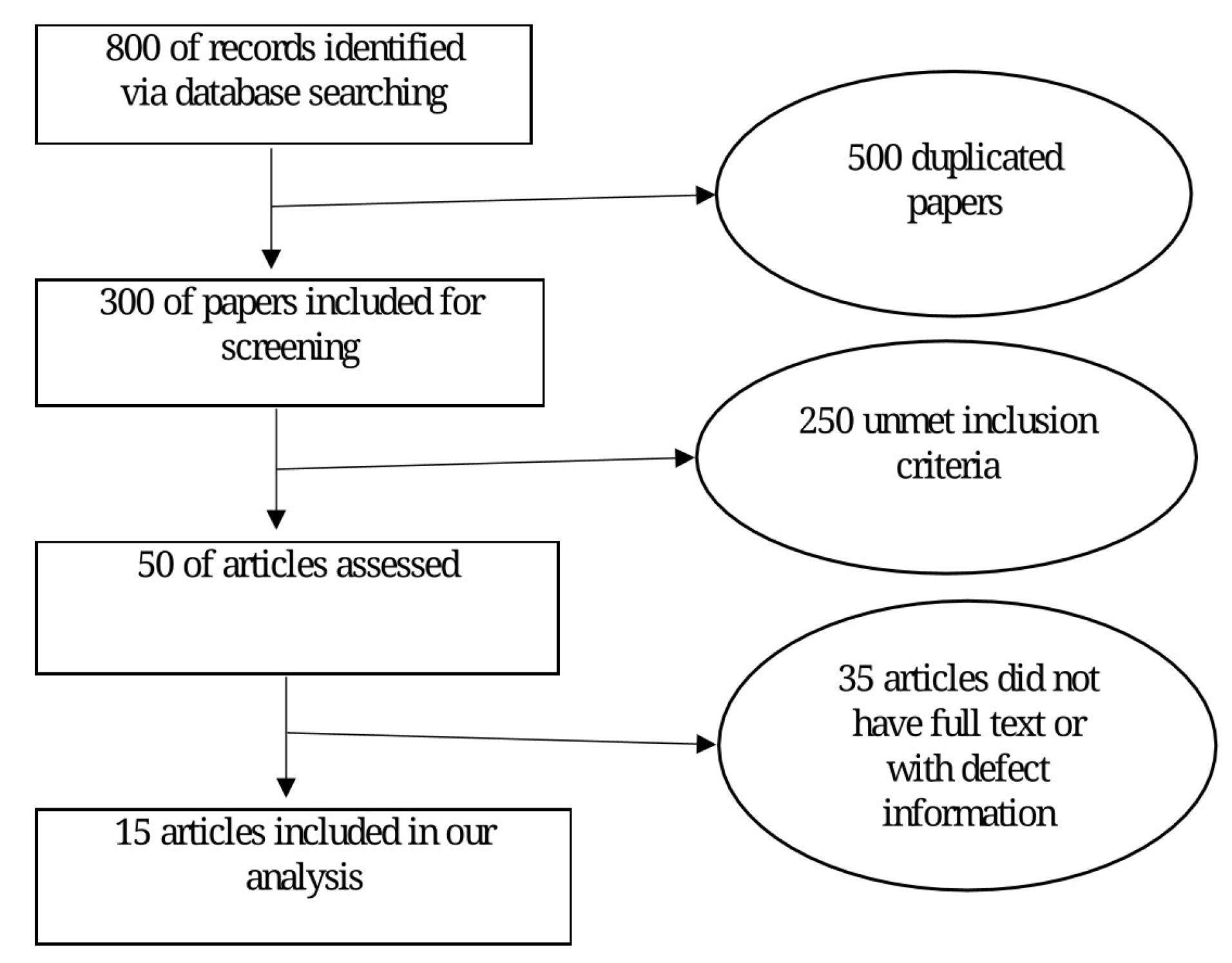
Figure 1.
Systematic Literature Review Process
.
Systematic Literature Review Process
All studies were conducted on the Iranian population between 2019 and 2024. Table 1 summarizes the key features of the reviewed articles.
Table 1.
Study Features
|
Authors
|
Year
|
Study Type
|
Place
|
Event
|
Sample Size
|
Age (Mean±SD)
|
Overall PTSD (%)
|
Mean (%)
|
Women (%)
|
| Abdollahzadeh et al28 |
2023 |
Cross-sectional study |
Mahabad |
Genital mutilation |
155 |
31.46 ± 6.94 |
3.9% |
- |
3.9% |
| Shabani et al19 |
2024 |
Cross-sectional study |
Lorestan, Khouzestan, Golestan |
Flood |
2305 |
36.8 ± 12.1 |
24.8% |
21.6% |
28% |
| Ahmadnejad et al23 |
2021 |
Cross-sectional study |
Baneh |
Childbirth |
365 |
28.0 ± 4.3 |
47.7% |
- |
47.7% |
| Hajizadeh et a24 |
2021 |
Prospective study |
Tabriz |
Childbirth |
288 |
26.0 ± 5.3 |
16.3% |
- |
16.3% |
| Ebrahimi et al13 |
2021 |
Cross-sectional study |
Shahroud |
Job |
228 |
34.03 ± 7.7 |
85.5% |
83.3% |
%87.7 |
| Hosseininejad et al12 |
2019 |
Cross-sectional study |
Mazandaran |
Job |
131 |
24.97 ± 2.6 |
82.41% |
82.96% |
82.08% |
| Hosseini et al20 |
2022 |
Cross-sectional study |
Sari |
COVID- 19 |
199 |
27.0 ± 4.3 |
19.1% |
0.5% |
18.6% |
| Bastami et al18 |
2024 |
Descriptive-analytical study |
Lorestan |
Flood |
470 |
32.25 ± 6.02 |
23.75% |
13.64% |
33.9% |
| Keyhani et al14 |
2023 |
Cross-sectional study |
Tehran |
Job |
365 |
34.06 ± 7.78 |
14.6% |
14.8% |
14.4% |
| Rostamizadeh et al17 |
2020 |
Retrospective cohort study |
Ilam |
War |
227 |
66.67 ± 7.16 |
16.3% |
14.3% |
18.3% |
| Sehat et al3 |
2020 |
Cross-sectional population-based study |
Kashan |
Trauma |
3880 |
30 ± 9 |
18.65% |
16% |
21.3% |
| Khademhamzehei et al21 |
2023 |
Cross-sectional study |
Hamadan |
COVID- 19 |
185 |
38.43 ± 14.07 |
63.5% |
63.8 |
63.2 |
| Khazaei et al15 |
2021 |
Cross-sectional study |
Hamadan |
Job |
259 |
28.88 ± 6.94 |
22% |
22% |
- |
| Sahebi et al16 |
2020 |
Systematic review and meta-analysis |
Iran |
Job |
274 |
35.21 ± 5.24 |
23.17% |
23.17% |
- |
| Faramarzi et al22 |
2023 |
Cross-sectional study |
Babol |
COVID-19 |
477 |
60.5 ± 17.9 |
8.1% |
- |
- |
Note. SD: Standard deviation; PTSD: Post-traumatic stress disorder.
Results indicate that the total sample size was 9868 participants, with a mean age of 35.61 ± 7.8 years. In this study, the I2 index for heterogeneity was 95.29. The meta-analysis was carried out through the random effects model due to the high and significant heterogeneity among the studies. According to the data analysis, the overall prevalence of PTSD was 31.87% (95% CI = 17.87- 45.87, I2 = 95.29%, P< 0.001) (Figure 2).
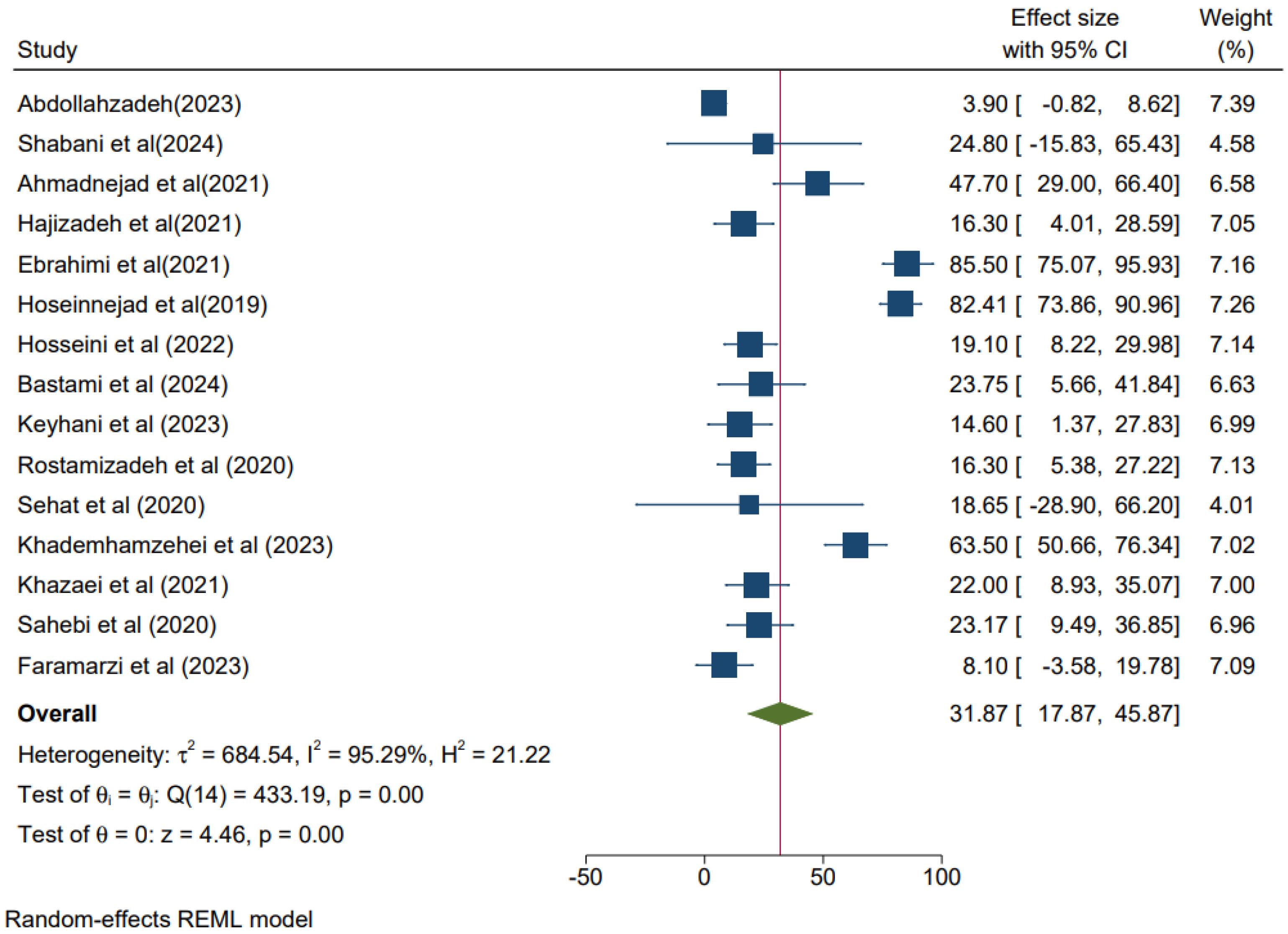
Figure 2.
Prevalence of Overall Post-traumatic Stress Disorder With a 95% Confidence Interval
.
Prevalence of Overall Post-traumatic Stress Disorder With a 95% Confidence Interval
Based on geographical region, the highest prevalence of PTSD was observed in Shahrood, Mazandaran, and Hamadan, respectively, which are located in different geographic regions of Iran, from north to east and west.
As seen in Figure 3, there is a significant relationship between PTSD prevalence in Iran and the year of the study (P = 0.04). Furthermore, although the prevalence of PTSD in Iran has decreased from 2019 to 2024, the change was not statistically significant. Additionally, metaregression results indicated no significant association between PTSD prevalence and study location or event type (P > 0.05).
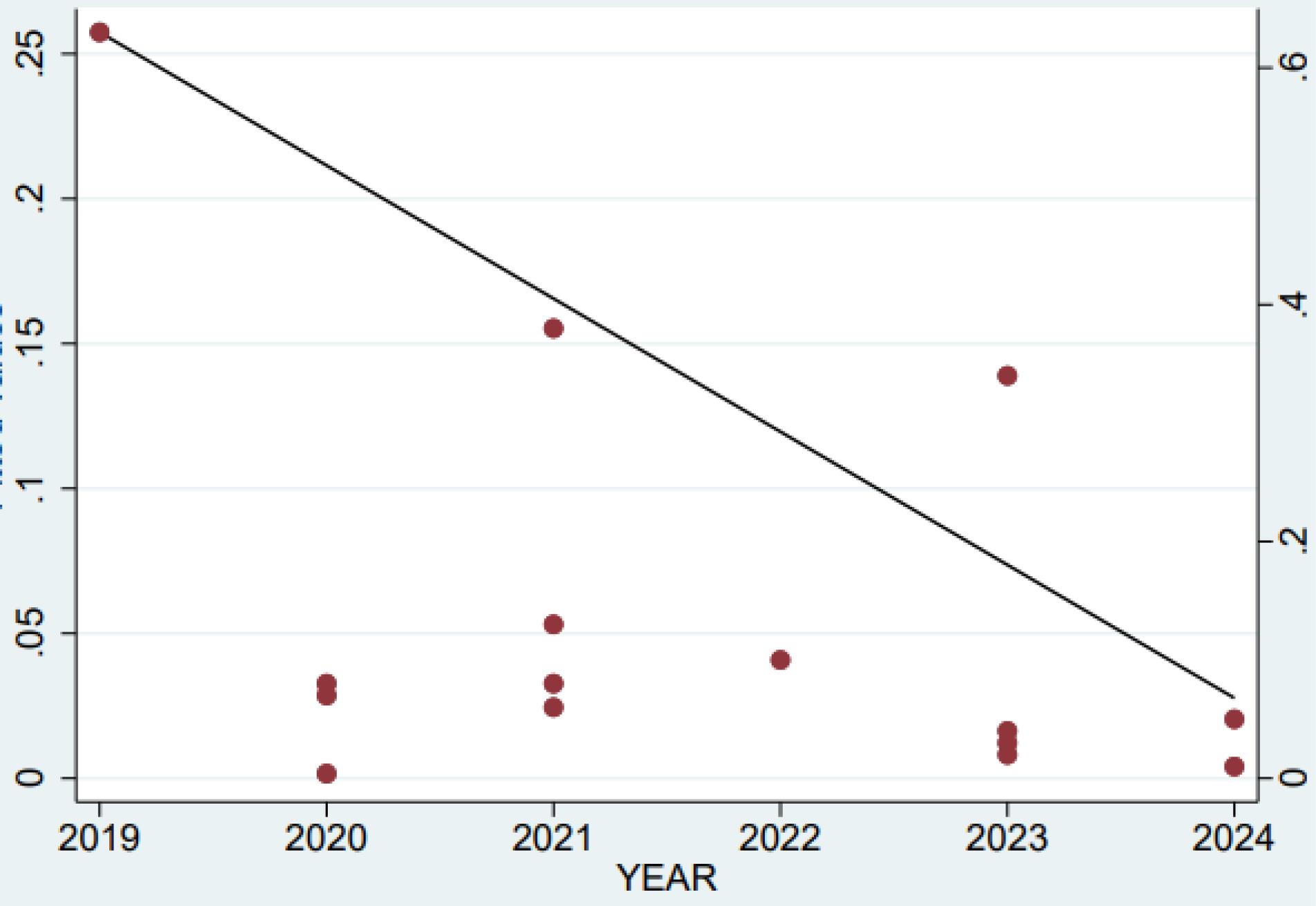
Figure 3.
Meta-Regression Analysis Based on the Year of Publication
.
Meta-Regression Analysis Based on the Year of Publication
Figures 4 and 5 show that the PTSD prevalence among Iranian men and women was 36.64% (95% CI = 19.17- 54.11, I2 = 94.57%) and 35.52% (95% CI = 18.55- 52.49, I2 = 96.06%), respectively.
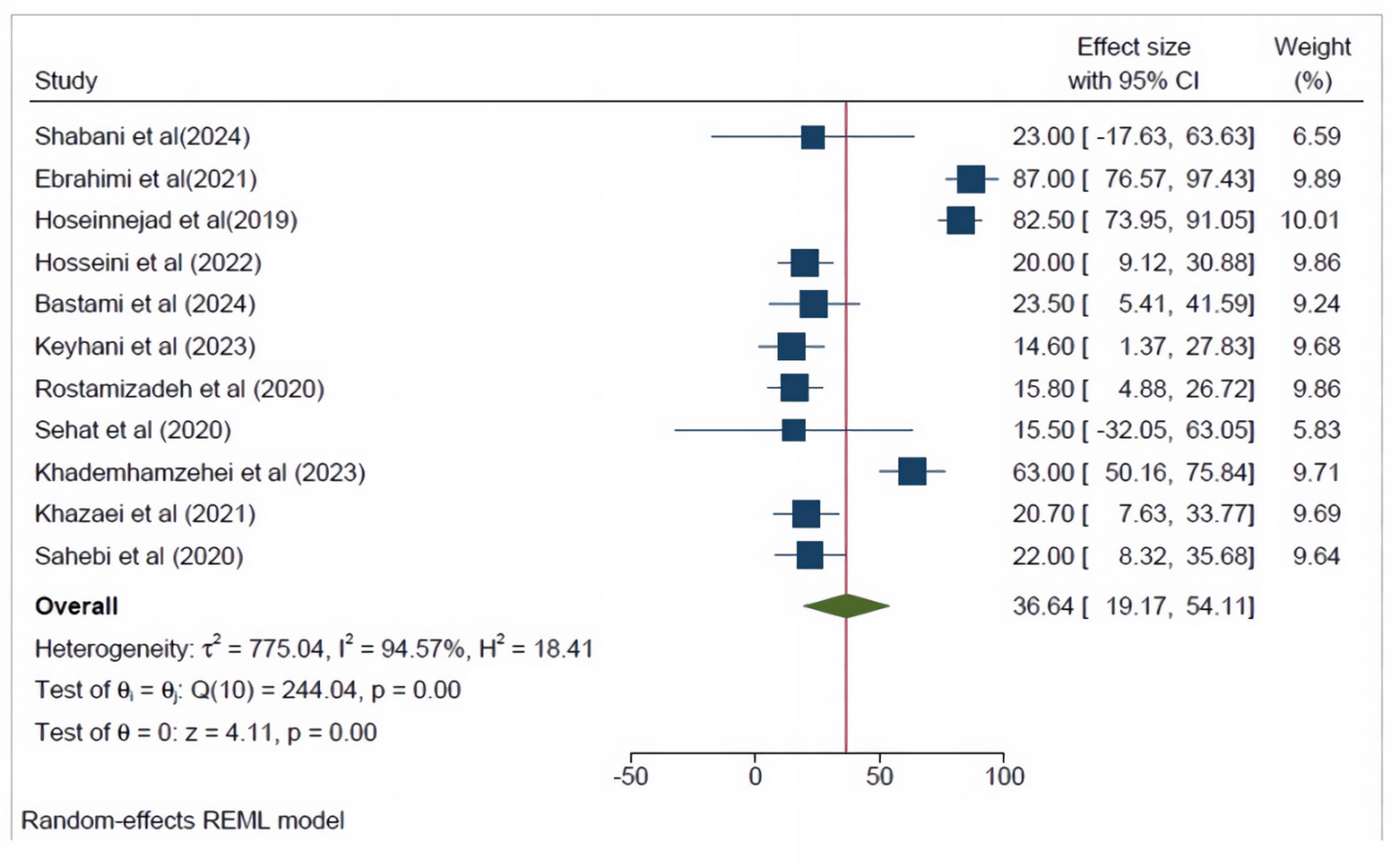
Figure 4.
Prevalence of Post-traumatic Stress Disorder in Men With 95% Confidence Interval
.
Prevalence of Post-traumatic Stress Disorder in Men With 95% Confidence Interval
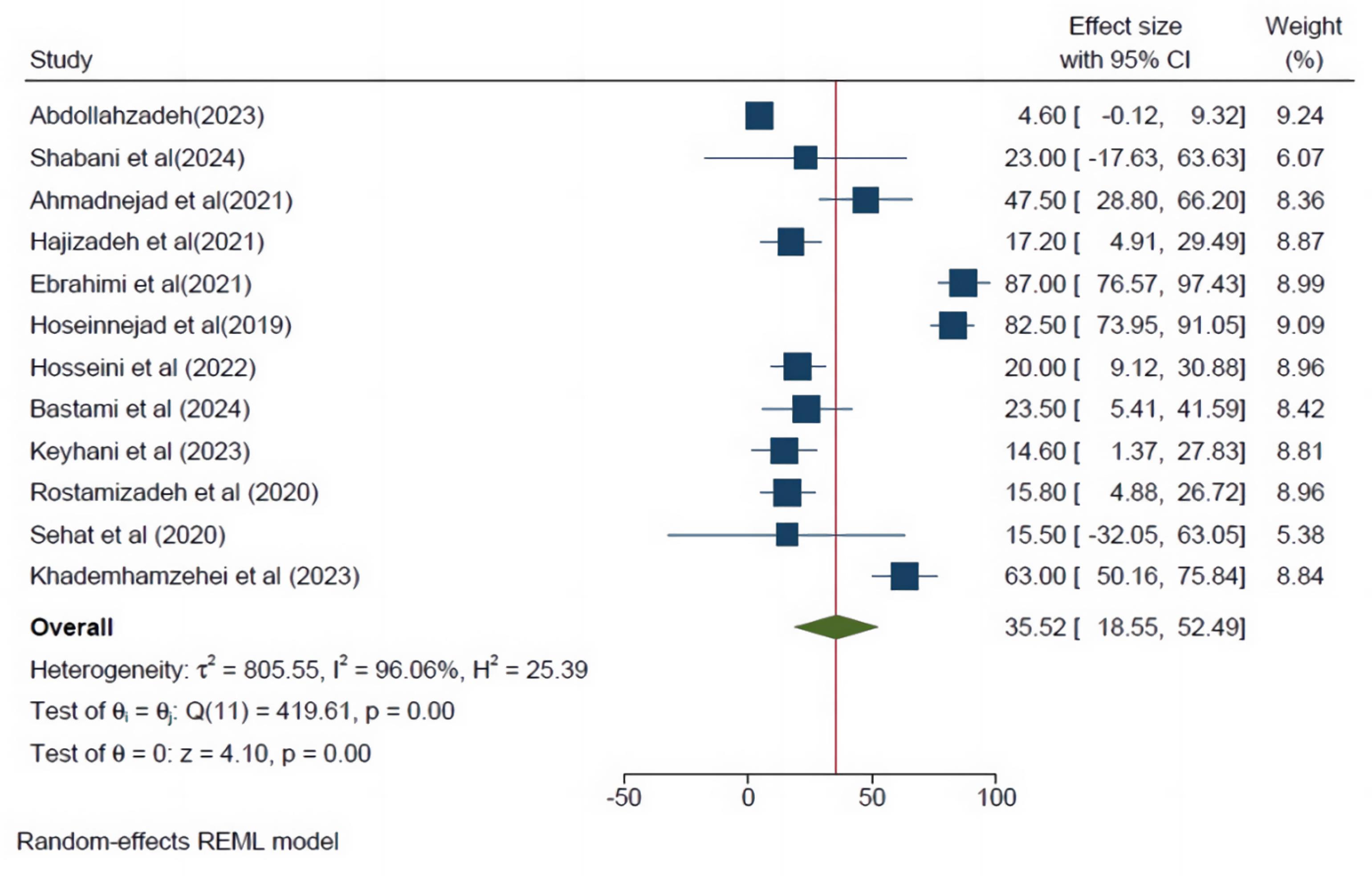
Figure 5.
Prevalence of Post-traumatic Stress Disorder in Women With 95% Confidence Interval
.
Prevalence of Post-traumatic Stress Disorder in Women With 95% Confidence Interval
Discussion
PTSD has been recognized as one of the most significant psychosocial consequences of trauma.29 This disorder affects the individual, social, and emotional dimensions of traumatic patients.30 Based on DSM-5, PTSD is categorized as “a disorder associated with trauma and stress, emerging following exposure to a traumatic event.” It is characterized by acute or chronic patterns.31
Various studies have reported the prevalence of PTSD in general populations in countries such as China,32 South Korea,33 Ethiopia,34 Lebanon,35 the USA,10 and England36; These figures were determined to be 53.2%, 26.8%, 37.3%, 33.3%, 26.9%, and 7.8%, respectively. Our study found that the overall PTSD prevalence in the Iranian population was 31.87%. These heterogeneous results may stem from different study methodologies, sample sizes, and the contextual personalities of participants. Additionally, the diversity in political, social, and cultural situations across countries may contribute to this discrepancy in the prevalence rates of PTSD.
Our meta-regression results indicated that the prevalence of PTSD in Iran has not decreased significantly from 2019 to 2024. Similar to other world countries, Iran experienced the COVID-19 pandemic during the last 5 years, which likely affected the prevalence of PTSD. Zhang et al37 found that PTSD prevalence during the COVID-19 pandemic in the general population was 15%. Another study in China reported that the PTSD prevalence is 4.6% in the general population and 25% in suspected or confirmed COVID-19 cases.38 Cook et al39 showed a PTSD prevalence of 23.88% during the COVID-19 pandemic. Furthermore, the results of a meta-analysis and systematic review conducted across 24 countries revealed that the overall PTSD prevalence in the general population is 17.52%.40
Initially, it was expected that the occurrence of a pandemic and its association with stressful events would intensify the level of PTSD. However, the existence of contradictory findings indicates that the prevalence of PTSD is not only dependent on the pandemic but is also influenced by other factors that need to be investigated in future studies.
The samples’ mean age was 35.61 ± 7.8 years, indicating a relatively young age. This finding is consistent with the studies by Scheeringa et al,41 Bastien et al,42 and Pasha et al.43 Young people are more involved in harmful behaviors and experience traumatic events than other age groups.
Another meta-analysis finding from our study reported that the prevalence of PTSD in Iranian men (36.64%) is higher than in women (35.52%). This finding contradicts previous Iranian studies by Merghati Khoei et al,44 Sepahvand et al,45 and Rafiey et al.46 These contradictory findings in Iranian studies highlight the need for conducting etiological studies in the future. Nevertheless, it is clear that Iranian men are more frequently exposed to unwanted events such as war, occupational incidents, and road traffic victims.
Conclusion
The main objective of our meta-analysis was to determine the prevalence of PTSD in the Iranian population from 2019 to 2024, which was found to be 31.87%, representing a relatively high level. Given the occurrence of natural disasters such as earthquakes, floods, and storms in Iran every year, alongside the high incidence of road traffic accidents, it is recommended that future studies assess PTSD prevalence and the trend of its changes over time. Unlike previous studies, our findings indicated that the prevalence of PTSD is higher among young Iranian men. Hence, social organizations and healthcare policymakers should focus on this age group.
Competing Interests
All authors declare no conflict of interests related to the publication process.
Ethical Approval
This study was extracted from the PhD thesis of the first author (Asad Imani). It was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences, under the ethical code: IR.AJUMS.REC.1403.284. We appreciate all the authors whose articles were used for analysis in this study.
Funding
This study was financially supported by the Research Deputy of Ahvaz Jundishapur University of Medical Sciences.
References
- Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA 2021; 325(18):1829-30. doi: 10.1001/jama.2021.5469 [Crossref] [ Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G. Trauma and PTSD in the WHO world mental health surveys. Eur J Psychotraumatol 2017; 8(Suppl 5):1353383. doi: 10.1080/20008198.2017.1353383 [Crossref] [ Google Scholar]
- Sehat Z, Fakharian E, Sehat M, Omidi A. Disability and post-trauma stress in the population over 15 years old in Kashan, Iran: a population-based study. Chin J Traumatol 2020; 23(6):351-5. doi: 10.1016/j.cjtee.2020.09.004 [Crossref] [ Google Scholar]
- Moradi S, Masjedi Arani A, Dolatshahi B, Saberi M, Shamsipour H. Prevalence of traumatic experiences and their relationship to mental health in Iranians. J Loss Trauma 2019; 24(8):691-705. doi: 10.1080/15325024.2019.1616923 [Crossref] [ Google Scholar]
- Isazadehfar K, Salamati P, Zafarghandi MR, Rahimi-Movaghar V, Khormali M, Baigi V. Insurance status and traumatized patients’ outcomes: a report from the national trauma registry of Iran. BMC Health Serv Res 2023; 23(1):392. doi: 10.1186/s12913-023-09369-9 [Crossref] [ Google Scholar]
- Roshanaei G, Khoshravesh S, Abdolmaleki S, Bathaei T, Farzian M, Saatian M. Epidemiological pattern of trauma patients based on the mechanisms of trauma: trends of a regional trauma center in Midwest of Iran. BMC Emerg Med 2022; 22(1):210. doi: 10.1186/s12873-022-00756-9 [Crossref] [ Google Scholar]
- Saberian L, Baigi V, Zafarghandi M, Naghdi K, Ozlaty M, Bahrami S. Gender-based trauma outcomes and predictors of postinjury in-hospital mortalities: a multicenter analysis from the national trauma registry of Iran. Arch Trauma Res 2021; 10(4):209-14. doi: 10.4103/atr.atr_64_21 [Crossref] [ Google Scholar]
- Thakur A, Choudhary D, Kumar B, Chaudhary A. A review on post-traumatic stress disorder (PTSD): symptoms, therapies and recent case studies. Curr Mol Pharmacol 2022; 15(3):502-16. doi: 10.2174/1874467214666210525160944 [Crossref] [ Google Scholar]
- Zalta AK, Tirone V, Orlowska D, Blais RK, Lofgreen A, Klassen B. Examining moderators of the relationship between social support and self-reported PTSD symptoms: a meta-analysis. Psychol Bull 2021; 147(1):33-54. doi: 10.1037/bul0000316 [Crossref] [ Google Scholar]
- Schein J, Houle C, Urganus A, Cloutier M, Patterson-Lomba O, Wang Y. Prevalence of post-traumatic stress disorder in the United States: a systematic literature review. Curr Med Res Opin 2021; 37(12):2151-61. doi: 10.1080/03007995.2021.1978417 [Crossref] [ Google Scholar]
- Yousefifard M, Ramezani F, Faridaalaee G, Baikpour M, Madani Neishaboori A, Vaccaro AR. Prevalence of post-traumatic stress disorder symptoms following traumatic spinal cord injury: a systematic review and meta-analysis. Harv Rev Psychiatry 2022; 30(5):271-82. doi: 10.1097/hrp.0000000000000340 [Crossref] [ Google Scholar]
- Hosseininejad SM, Jahanian F, Elyasi F, Mokhtari H, Eslami Koulaei M, Pashaei SM. The prevalence of post-traumatic stress disorder among emergency nurses: a cross-sectional study in northern Iran. Biomedicine (Taipei) 2019; 9(3):19. doi: 10.1051/bmdcn/2019090319 [Crossref] [ Google Scholar]
- Ebrahimi H, Mirhosseini S, Basirinezhad MH, Shariati E. Prevalence of post-traumatic stress disorder (PTSD) following COVID-19 epidemic in health workers of Shahroud University of Medical Sciences. Avicenna J Nurs Midwifery Care 2021; 29(4):340-8. doi: 10.30699/ajnmc.29.4.340 [Crossref] [ Google Scholar]
- Keyhani A, Rahnejat AM, Dabaghi P, Taghva A, Ebrahimi MR, Nezami Asl A. Prevalence of post-traumatic stress disorder among the healthcare workers involved with COVID-19 treatment and its effective factors in military hospitals of Iran. Iran J War Public Health 2023; 15(1):61-6. doi: 10.58209/ijwph.15.1.61 [Crossref] [ Google Scholar]
- Khazaei A, Navab E, Esmaeili M, Masoumi H. Prevalence and related factors of post-traumatic stress disorder in emergency medical technicians; a cross-sectional study. Arch Acad Emerg Med 2021; 9(1):e35. doi: 10.22037/aaem.v9i1.1157 [Crossref] [ Google Scholar]
- Sahebi A, Yousefi K, Moayedi S, Golitaleb N, Esmaeili Vardanjani A, Golitaleb M. Prevalence of post-traumatic stress disorder among firefighters in Iran: a systematic review and meta-analysis. Iran J Psychiatry 2020; 15(4):358-65. doi: 10.18502/ijps.v15i4.4301 [Crossref] [ Google Scholar]
- Rostamizadeh A, Abolfathi Momtaz Y, Foroughan M. Rate and associated factors of post-traumatic stress disorder in elderly survivors of bombardment in Ilam city, Iran. Iran J War Public Health 2020; 12(2):125-32. doi: 10.29252/ijwph.12.2.125 [Crossref] [ Google Scholar]
- Bastami F, Mohammadi R, Asadi Piri Z, Valipour E, Ahmadi P, Almasian M. Prevalence of post-traumatic stress disorder and its relationship with coping strategies among flood victims: evidence from Iran. J Affect Disord Rep 2024; 15:100704. doi: 10.1016/j.jadr.2023.100704 [Crossref] [ Google Scholar]
- Shabani A, Rasoulian M, Naserbakht M, Hakim Shooshtari M, Hajebi A, Tiyuri A. Prevalence and determinants of post-traumatic stress disorder five months after the 2019 huge flooding in Iran. BMC Public Health 2024; 24(1):346. doi: 10.1186/s12889-024-17861-y [Crossref] [ Google Scholar]
- Hosseini SH, Elyasi F, Moosazadeh M, Ghafour I. Evaluation of the frequency of post-traumatic stress disorder in patients with COVID-19 admitted to hospitals in Sari, Iran in 2020. Iran J Psychiatry Behav Sci 2022; 16(1):e115663. doi: 10.5812/ijpbs.115663 [Crossref] [ Google Scholar]
- Khademhamzehei E, Mortazavi Z, Najafi-Vosough R, Haghgoo H, Mortazavi SS. The post-traumatic stress disorder in COVID-19 recovered patients: a cross-sectional study. Archives of Rehabilitation 2023; 24(1):28-41. doi: 10.32598/rj.24.1.3011.4 [Crossref] [ Google Scholar]
- Faramarzi M, Chehrazi M, Kheirkhah F, Hamidia A, Gheisari F, Khoozan M. Prevalence of psychological distress and post-traumatic stress symptoms and associated factors in hospitalized Iranian COVID-19 patients. Oman Med J 2023; 38(2):e480. doi: 10.5001/omj.2023.59 [Crossref] [ Google Scholar]
- Ahmadnejad R, Malakouti J, Mirghafourvand M, Farshbaf Khalili A. The prevalence of post-traumatic stress disorder following childbirth and its predictors in Iranian women. Shiraz E Med J 2021; 22(9):e107304. doi: 10.5812/semj.107304 [Crossref] [ Google Scholar]
- Hajizadeh K, Mirghafourvand M. Relationship of post-traumatic stress disorder with disrespect and abuse during childbirth in a group of Iranian postpartum women: a prospective study. Ann Gen Psychiatry 2021; 20(1):8. doi: 10.1186/s12991-021-00331-9 [Crossref] [ Google Scholar]
- Frew E, Breheny K. Health economics methods for public health resource allocation: a qualitative interview study of decision makers from an English local authority. Health Econ Policy Law 2020; 15(1):128-40. doi: 10.1017/s174413311800052x [Crossref] [ Google Scholar]
- Alipour F, Ahmadi S. Social support and post-traumatic stress disorder (PTSD) in earthquake survivors: a systematic review. Soc Work Ment Health 2020; 18(5):501-14. doi: 10.1080/15332985.2020.1795045 [Crossref] [ Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370(9596):1453-7. doi: 10.1016/s0140-6736(07)61602-x [Crossref] [ Google Scholar]
- Abdollahzadeh M, Nourizadeh R, Sattarzadeh Jahdi N. Post-traumatic stress disorder among Iranian women with genital mutilation: a cross-sectional study. Reprod Health 2023; 20(1):59. doi: 10.1186/s12978-022-01561-0 [Crossref] [ Google Scholar]
- Wang Y, Chung MC, Wang N, Yu X, Kenardy J. Social support and post-traumatic stress disorder: a meta-analysis of longitudinal studies. Clin Psychol Rev 2021; 85:101998. doi: 10.1016/j.cpr.2021.101998 [Crossref] [ Google Scholar]
- Couette M, Mouchabac S, Bourla A, Nuss P, Ferreri F. Social cognition in post-traumatic stress disorder: A systematic review. Br J Clin Psychol 2020; 59(2):117-38. doi: 10.1111/bjc.12238 [Crossref] [ Google Scholar]
- Pai A, Suris AM, North CS. Post-traumatic stress disorder in the DSM-5: controversy, change, and conceptual considerations. Behav Sci (Basel) 2017; 7(1):7. doi: 10.3390/bs7010007 [Crossref] [ Google Scholar]
- Mao J, Wang C, Teng C, Wang M, Zhou S, Zhao K. Prevalence and associated factors of PTSD symptoms after the COVID-19 epidemic outbreak in an online survey in China: the age and gender differences matter. Neuropsychiatr Dis Treat 2022; 18:761-71. doi: 10.2147/ndt.s351042 [Crossref] [ Google Scholar]
- Yang HJ, Jung YE, Park JH, Kim MD. Prevalence and associated factors of post-traumatic stress disorder in Gangjeong village residents, Jeju-do. J Korean Neuropsychiatr Assoc 2019; 58(4):314-21. doi: 10.4306/jknpa.2019.58.4.314 [Crossref] [ Google Scholar]
- Asnakew S, Shumet S, Ginbare W, Legas G, Haile K. Prevalence of post-traumatic stress disorder and associated factors among Koshe landslide survivors, Addis Ababa, Ethiopia: a community-based, cross-sectional study. BMJ Open 2019; 9(6):e028550. doi: 10.1136/bmjopen-2018-028550 [Crossref] [ Google Scholar]
- Farhood LF, Dimassi H. Prevalence and predictors for post-traumatic stress disorder, depression and general health in a population from six villages in South Lebanon. Soc Psychiatry Psychiatr Epidemiol 2012; 47(4):639-49. doi: 10.1007/s00127-011-0368-6 [Crossref] [ Google Scholar]
- Lewis SJ, Arseneault L, Caspi A, Fisher HL, Matthews T, Moffitt TE. The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. Lancet Psychiatry 2019; 6(3):247-56. doi: 10.1016/s2215-0366(19)30031-8 [Crossref] [ Google Scholar]
- Zhang L, Pan R, Cai Y, Pan J. The prevalence of post-traumatic stress disorder in the general population during the COVID-19 pandemic: a systematic review and single-arm meta-analysis. Psychiatry Investig 2021; 18(5):426-33. doi: 10.30773/pi.2020.0458 [Crossref] [ Google Scholar]
- Sun L, Sun Z, Wu L, Zhu Z, Zhang F, Shang Z. Prevalence and risk factors for acute post-traumatic stress disorder during the COVID-19 outbreak. J Affect Disord 2021; 283:123-9. doi: 10.1016/j.jad.2021.01.050 [Crossref] [ Google Scholar]
- Cooke JE, Eirich R, Racine N, Madigan S. Prevalence of post-traumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatry Res 2020; 292:113347. doi: 10.1016/j.psychres.2020.113347 [Crossref] [ Google Scholar]
- Yunitri N, Chu H, Kang XL, Jen HJ, Pien LC, Tsai HT. Global prevalence and associated risk factors of post-traumatic stress disorder during COVID-19 pandemic: a meta-analysis. Int J Nurs Stud 2022; 126:104136. doi: 10.1016/j.ijnurstu.2021.104136 [Crossref] [ Google Scholar]
- Scheeringa MS. Development of a brief screen for symptoms of post-traumatic stress disorder in young children: the young child PTSD screen. J Dev Behav Pediatr 2019; 40(2):105-11. doi: 10.1097/dbp.0000000000000639 [Crossref] [ Google Scholar]
- John-Baptiste Bastien R, Jongsma HE, Kabadayi M, Billings J. The effectiveness of psychological interventions for post-traumatic stress disorder in children, adolescents and young adults: a systematic review and meta-analysis. Psychol Med 2020; 50(10):1598-612. doi: 10.1017/s0033291720002007 [Crossref] [ Google Scholar]
- Pasha H, Omidvar S, Faramarzi M, Bakhtiari A. Depression, anxiety, stress, and PTSD symptoms during the first and second COVID-19 waves: a comparison of elderly, middle-aged, and young people in Iran. BMC Psychiatry 2023; 23(1):190. doi: 10.1186/s12888-023-04677-0 [Crossref] [ Google Scholar]
- Merghati Khoei E, Rezaei Z, Mohraz M, Brady KT, Killeen T, Korte JE. Gender differences in post-traumatic stress disorder and depression among Iranian population with substance use disorder. J Subst Use 2023; 28(3):425-30. doi: 10.1080/14659891.2022.2051624 [Crossref] [ Google Scholar]
- Sepahvand H, Mokhtari Hashtjini M, Salesi M, Sahraei H, Pirzad Jahromi G. Prevalence of post-traumatic stress disorder (PTSD) in Iranian population following disasters and wars: a systematic review and meta-analysis. Iran J Psychiatry Behav Sci 2019; 13(1):e66124. doi: 10.5812/ijpbs.66124 [Crossref] [ Google Scholar]
- Rafiey H, Alipour F, LeBeau R, Salimi Y. Prevalence and determinants of PTSD 3 years after an earthquake in Iran. Community Ment Health J 2019; 55(3):542-7. doi: 10.1007/s10597-019-00384-x [Crossref] [ Google Scholar]