Arch Iran Med. 26(9):542-546.
doi: 10.34172/aim.2023.79
Case Report
Intramural Gastric Abscess Misdiagnosed as Advanced Gastric Cancer
Na-Ri Lee Resources, Software, Writing – original draft, 1, 2 
Eun-Kee Song Data curation, Formal analysis, Investigation, Visualization, 1, 2 
So-Yeon Jeon Conceptualization, Methodology, Project administration, Supervision, Validation, Writing – review & editing, 1, 2, * 
Author information:
1Division of Oncology and Hematology, Department of Internal Medicine, Jeonbuk National University Hospital-Jeonbuk National University Medical School, Jeonju, Republic of Korea
2Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Republic of Korea
Abstract
An intramural gastric abscess is a rare condition often mistaken for other medical diseases such as gastric cancer and neoplasms. We present a case of a patient initially believed to have pancreatic cancer based on his computed tomography scan. The clinical diagnosis of locally advanced gastric cancer was made on subsequent magnetic resonance cholangiography and endoscopic ultrasound (EUS). However, several EUS-guided biopsies did not reveal malignant cells. A partial gastrectomy was performed for diagnostic and therapeutic purposes. The specimen showed only inflammatory cells, without any malignant cells. The final diagnosis was gastric wall abscess (GWA) that infiltrated and adhered to the adjacent tissues. This case reminds that physicians should include GWA as a differential diagnosis in the suspicion of gastric cancer. Although GWA is rare, it is often forgotten when focusing on the possibility of fatal cancer.
Keywords: Case report, Gastric cancer, Gastric wall abscess, Surgery
Copyright and License Information
© 2023 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Lee NR, Song EK, Jeon SY. Intramural gastric abscess misdiagnosed as advanced gastric cancer. Arch Iran Med. 2023;26(9):542-546. doi: 10.34172/aim.2023.79
Introduction
An intramural gastric abscess is a rare condition that may be difficult to diagnose based on imaging alone. Gastric wall abscesses (GWAs) are often misdiagnosed as stomach cancers.1‒3 GWA can be easily diagnosed with a secreting mass on endoscopy. However, in the absence of such discharge, diagnosis may be difficult, even after various imaging tests. Even if the discharge is present, its diagnosis may be difficult if other imaging studies consistently suggest malignancy. We report a case of GWA initially considered to be a pancreatic tail cancer directly invading the gastric wall, based on initial radiologic imaging.
Case Report
A 60-year-old man presented to our institution with abdominal pain, characterized as stabbing in nature, radiating from the epigastrium to the back. Although the patient did not recall his previous weight, he allegedly had significant weight loss.
His abdominal pain began several weeks prior to admission. Abdominopelvic computed tomography (AP-CT) performed at the previous hospital indicated suspected pancreatic cancer. The patient was transferred to our hospital for diagnosis and treatment.
The patient was diabetic and hypertensive. Five years prior, he had undergone extracorporeal shockwave lithotripsy for pancreatic duct stones. He was a regular alcoholic beverage drinker, consuming one or two cups of kaoliang 20 times a month for 30 years. His father died of gastric cancer several years ago.
On physical examination, he had a body temperature of 36.9 °C, resting respiratory rate of 20 breaths/min, heart rate of 78 bpm, and blood pressure of 140/89 mm Hg. No abdominal or rebound tenderness was found.
Laboratory examination revealed the following results: white blood cell count of 8390/mm3 (reference range [RR]: 3.5‒10.5 × 103/mm3); hemoglobin of 12.0 g/dL; hematocrit of 34.5%; and platelet count of 267 × 103/µL. His erythrocyte sedimentation rate was 98 mm/h (RR, < 9 mm/h), and his high-sensitivity C-reactive protein level was 130.47 mg/L (RR, < 5 mg/L). His CA 19‒9 level was 4.15 U/mL (RR, < 37.0 U/mL).
AP-CT, performed in another hospital, revealed a pancreatic mass, measuring approximately 7 × 4.5 cm, that directly invaded the gastric wall. The mass was suspected to be a pancreatic malignancy (Figure 1). Magnetic resonance cholangiopancreatography (MRCP) was performed to localize the mass. MRCP showed irregular wall thickening of more than 5 cm in length along the lesser curvature of the stomach. The mucosal layer was almost maintained, and the wall thickening inside was observed as low density (Figure 2). Cystic or necrotic portions had invaded the splenic vessels behind the pancreas. The main mass abutted the pancreas; however, the pancreatic duct appeared intact, possibly indicating that the tumor mass did not originate from the pancreatic duct. Numerous enlarged lymph nodes were observed in the periportal and para-aortic areas; however, their size was too small for characterization. MRCP concluded that the malignant-appearing gastric mass had a retropancreatic extension.
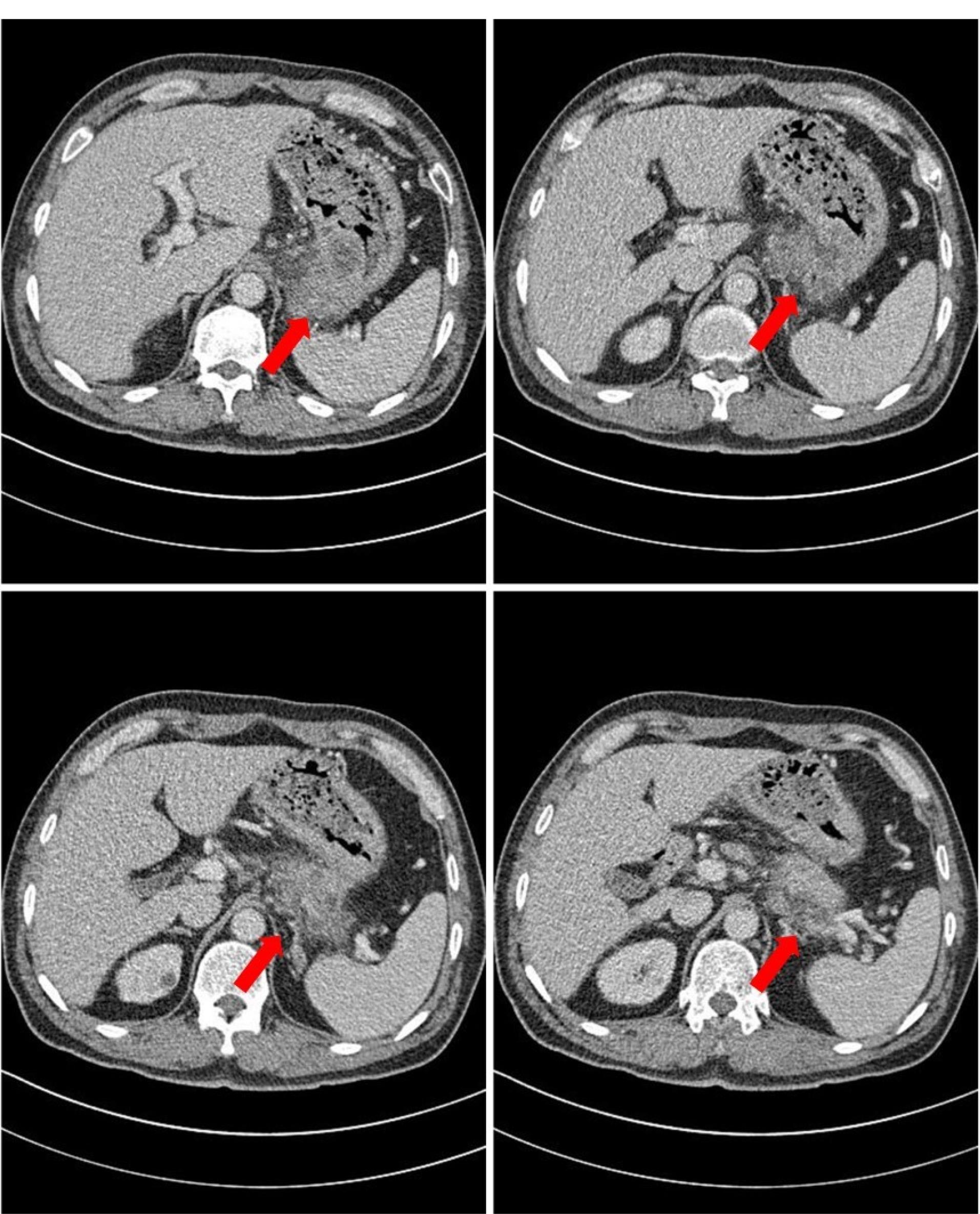
Figure 1.
Abdominopelvic computed tomography (AP-CT) Performed at the Local Clinic. Pancreatic mass measuring approximately 7 × 4.5 cm and directly invading the gastric wall was observed, leading to a high suspicion of cancer
.
Abdominopelvic computed tomography (AP-CT) Performed at the Local Clinic. Pancreatic mass measuring approximately 7 × 4.5 cm and directly invading the gastric wall was observed, leading to a high suspicion of cancer
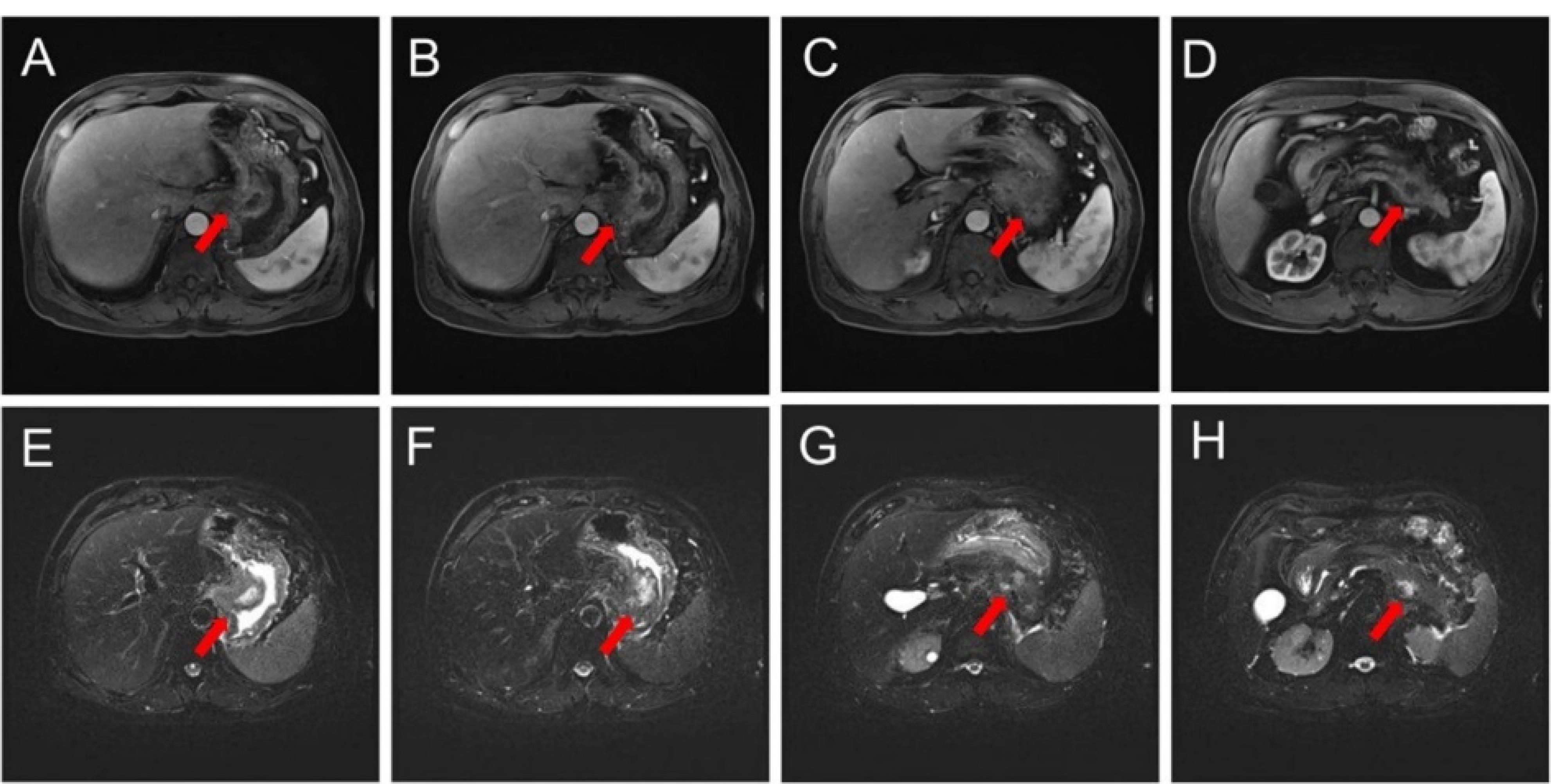
Figure 2.
Magnetic Resonance Cholangiopancreatography (MRCP) With Enhancement. A-D. T1-weighted images. E-H. T2-weighted images. MRCP shows irregular wall thickening along the lesser curvature of the upper body of the stomach. The mass abutted the pancreas; however, the mass was not considered to originate from pancreatic ductal cancer
.
Magnetic Resonance Cholangiopancreatography (MRCP) With Enhancement. A-D. T1-weighted images. E-H. T2-weighted images. MRCP shows irregular wall thickening along the lesser curvature of the upper body of the stomach. The mass abutted the pancreas; however, the mass was not considered to originate from pancreatic ductal cancer
Upper esophagogastroduodenoscopy (EGD) revealed erythematous bulging mucosa at the gastric fundus, oozing with whitish pus-like fluid (Figure 3). The endoscopist suggested the presence of gastric cancer or an inflammatory mass. We performed endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) and core needle biopsies. On EUS, we observed a gastric fundal wall mass measuring approximately 3 cm, with coarse echogenicity (Figure 3). Peripancreatic and retropancreatic masses > 3 cm in size were also observed, showing mixed echogenicity with irregular margins. Based on EUS findings, gastric cancer with retroperitoneum, splenic vein, and pancreatic invasion, with abscess formation in the gastric wall, was suspected. At this point, the differential diagnoses included retroperitoneal cancer with stomach invasion, pancreatic cancer with stomach invasion, and inflammatory masses of the stomach and retroperitoneum, in order of decreasing probability. Only acute suppurative inflammatory cells were observed on both FNA cytology and biopsies of the pancreas and stomach. A repeat EUS was performed, and FNA cytology and biopsies were consistent with an abscess in both the gastric wall and the pancreas. Because cancer could not be completely ruled out, a laparoscopic biopsy was performed. Preoperative AP-CT revealed that the mass volume had decreased to less than 2 cm, and the retropancreatic extension had markedly improved (Figure 4). Intraoperatively, adhesions were observed between the lower curvature of the stomach and the tail of the pancreas. There was no palpable hard mass suggesting malignancy. The adhesions were severe, so dissection was impossible, and we switched from laparoscopic to open surgery. The midbody of the stomach was removed by wedge resection, and the tail of the pancreas that adhered to the stomach was removed. All the specimens showed chronic inflammation without any malignant cells. The final diagnosis was GWA with pancreatic and retroperitoneal infiltrations.
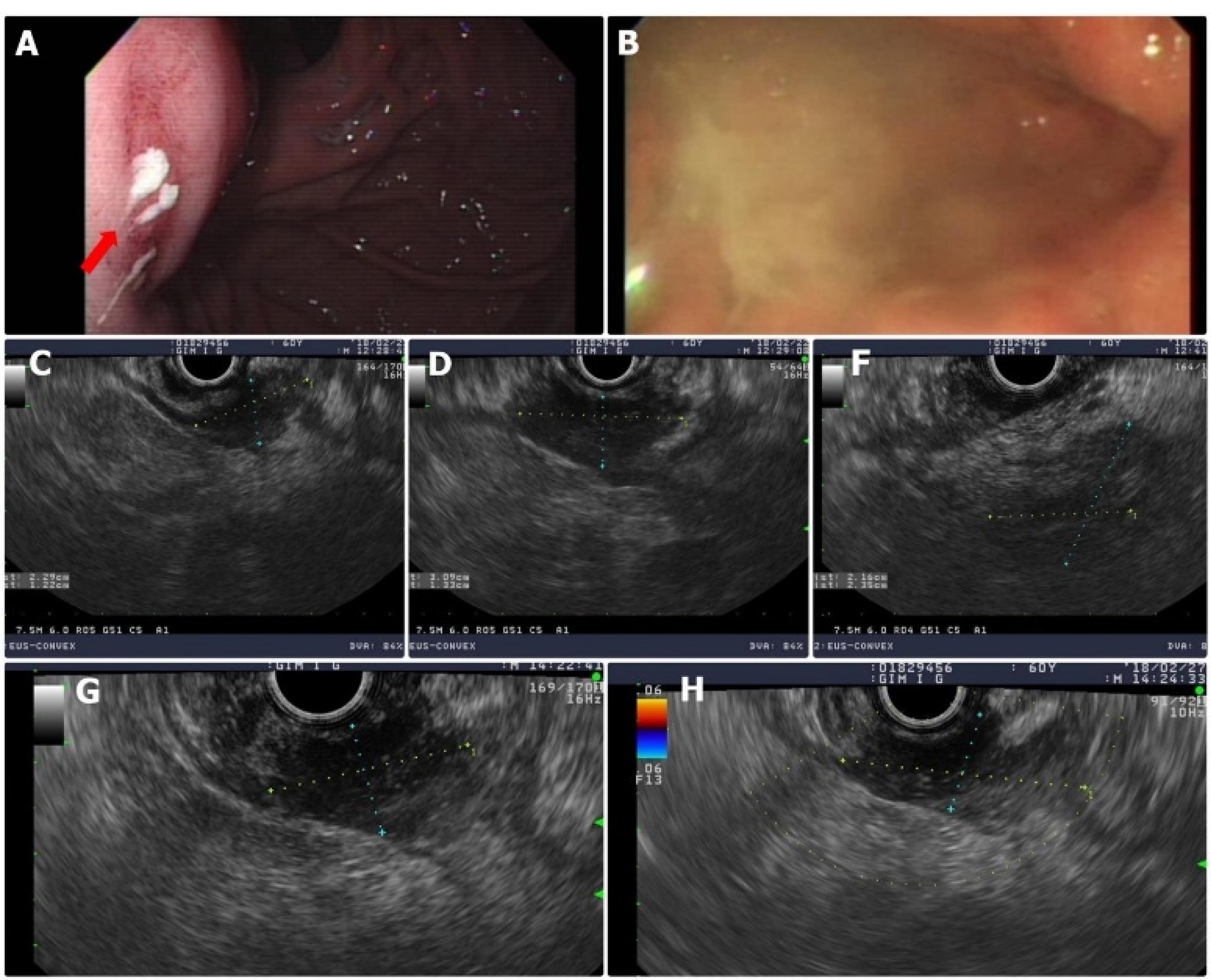
Figure 3.
Endoscopic ultrasound (EUS) Showing an Approximately 3 cm-Sized Mass in the Gastric Fundal Wall. A-B. After EUS-guided fine needle aspiration, a whitish discharge oozed from the biopsy site. C-G. A mixed echoic mass measuring larger bigger than 3 cm with an irregular margin was noted. Gastric cancer was suggested based on EUS. Other possible diagnoses included retroperitoneal cancer, pancreatic cancer, and inflammatory mass of the stomach and retroperitoneum
.
Endoscopic ultrasound (EUS) Showing an Approximately 3 cm-Sized Mass in the Gastric Fundal Wall. A-B. After EUS-guided fine needle aspiration, a whitish discharge oozed from the biopsy site. C-G. A mixed echoic mass measuring larger bigger than 3 cm with an irregular margin was noted. Gastric cancer was suggested based on EUS. Other possible diagnoses included retroperitoneal cancer, pancreatic cancer, and inflammatory mass of the stomach and retroperitoneum
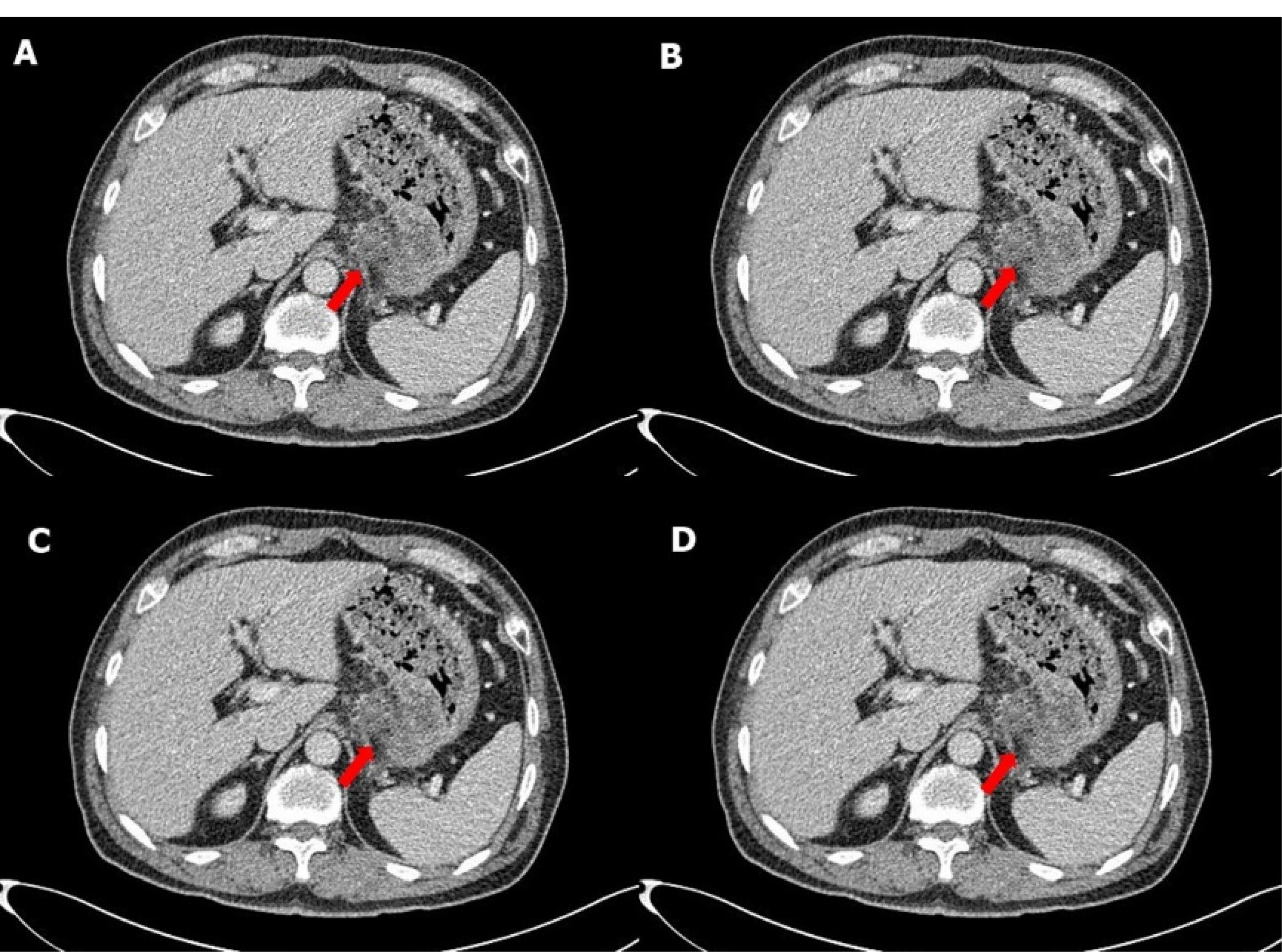
Figure 4.
Follow-up Abdominopelvic Computed Tomography Showing a Decrease in Mass Volume by < 2 cm and Improvement in Retropancreatic Wall Extension
.
Follow-up Abdominopelvic Computed Tomography Showing a Decrease in Mass Volume by < 2 cm and Improvement in Retropancreatic Wall Extension
No antibiotics were administered because there were no clinical signs suggesting infection at the time of admission. However, prophylactic antibiotic (ceftezole 1 g every 12 h) was initiated preoperatively. The patient recovered well, without any signs of inflammation, and was discharged. On his outpatient follow-up visit, the patient remains in good health.
Discussion
GWA is a rare variant of suppurative gastritis. The diagnosis of GWA is made with the presence of an abscess with suppurative pus discharge. However, this finding is also present in other medical conditions, such as several types of subepithelial gastric neoplasms, lipomas, and hematomas. When an abscess directly invades adjacent organs, it can be confused with gastric cancer, gastrointestinal stromal tumors (GISTs), and neuroendocrine neoplasms.2 Therefore, early diagnosis of GWA is difficult, and as a result, its mortality rate is high.4 GWA diagnosis depends on a series of imaging examinations. EGD, CT, and EUS are crucial for distinguishing between gastric cancer and abscess.1 In the present case, the mass was misdiagnosed as pancreatic cancer on the initial AP-CT. However, MRCP suggested a diagnosis of gastric cancer with pancreatic and retroperitoneal infiltrations. On EUS, masses larger than 3 cm were observed in the gastric wall, pancreas, and retroperitoneum. Therefore, EUS findings suggested gastric cancer accompanied by gastric abscess and retroperitoneal invasion. GWA generally shows a thickened wall with a localized hypoechoic mass, which has heterogeneous echogenicity, mainly fluid echo and few gas or foreign body echoes in the muscular or submucosal layer on EUS.4 Serial MRCP and EUS examinations helped change our patient’s diagnosis from pancreatic cancer to gastric cancer, but did not raise the suspicion of GWA. Even though pus secretion, the most common diagnostic finding, was seen on EGD, it was thought to be a malignant tumor accompanied by abscesses. This is because there have been case reports of GWA associated with GIST or gastric cancer.
5‒7 Since we could not obtain any malignant tissues, we decided to perform surgical resection for pathological confirmation and treatment. The radiologist interpreted the preoperative AP-CT as fluid collection accompanied by pancreatitis because the lesion was reduced to less than 2 cm and showed improvement. However, since malignancy was highly suspected, we ignored the possibility of benign disease.
The mortality rate of GWA has decreased from 92% to 33%,8 due to advances in surgical resection and antibiotic treatment. The treatment success rate is higher in patients treated with surgical resection plus medical antibiotic therapy than those treated with only medical antibiotics. Surgical resection and antibiotic therapy are the mainstream treatments; however, surgical approaches probably result from the fact that GWA is difficult to diagnose preoperatively and is often misdiagnosed as a more common surgical problem, such as gastric cancer or stromal tumors.8‒11 Recently, therapeutic endoscopic interventions such as endoscopic and percutaneous drainage with antibiotic therapy have been attempted to replace surgery.2,12 However, when the disease is recurrent or complicated by stromal tumors, surgical treatment is needed.2 In the present case, we believe that the patient would eventually have to undergo surgery because GWA was complicated by infiltrating adjacent organs. Surgery allows accurate diagnosis and treatment at the same time and effectively lowers the mortality rate; therefore, surgery is still the mainstream treatment.
Conclusion
GWA is a rare condition which is sometimes difficult to diagnose radiologically. Most often, GWA is mistaken for gastric cancer. We report a case of a gastric abscess mimicking pancreatic cancer on initial radiological imaging. A series of imaging studies have suggested that the diagnosis is locally advanced gastric cancer. Even when pus discharge, the most diagnostic feature of GWA, was seen on EGD, concerns about malignant tumors continued to be intensively expressed. GWA was diagnosed and treated with open surgery followed by antibiotics. This case reminds physicians not to ignore or overlook the possibility of GWA owing to its rarity, even though it has typical clinical features, while focusing on the deadly cancer disease.
Competing Interests
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the Institutional Review Board of Jeonbuk National University Hospital (IRB Ref No: CUH 2020-11-022). The need for informed consent was waived by the Institutional Review Board. The patient in the case was no longer visiting the hospital, written consent could not be obtained, and IRB approval was obtained to waive from the informed consent.
Funding
The authors received no financial support for the research, authorship, or publication of this article.
References
- Chen Y, Han Y, Du J. Diagnostic challenges in differentiating intramural gastric abscess from gastric cancer: two case reports. Medicine (Baltimore) 2018; 97(43):e12756. doi: 10.1097/md.0000000000012756 [Crossref] [ Google Scholar]
- Chen CH, Yang CC, Yeh YH, Hwang MH. Gastric wall abscess presenting as a submucosal tumor: case report. Gastrointest Endosc 2003; 57(7):959-62. doi: 10.1016/s0016-5107(03)70053-4 [Crossref] [ Google Scholar]
- Bodnár Z, Bubán T, Várvölgyi C. Submucosal tumor-like gastric wall abscess. Gastrointest Endosc 2004; 59(4):599. doi: 10.1016/s0016-5107(03)02724-x [Crossref] [ Google Scholar]
- Kim SB, Oh MJ, Lee SH. Gastric subepithelial lesion complicated with abscess: case report and literature review. World J Gastroenterol 2015; 21(20):6398-403. doi: 10.3748/wjg.v21.i20.6398 [Crossref] [ Google Scholar]
- Osada T, Nagahara A, Kodani T, Namihisa A, Kawabe M, Yoshizawa T. Gastrointestinal stromal tumor of the stomach with a giant abscess penetrating the gastric lumen. World J Gastroenterol 2007; 13(16):2385-7. doi: 10.3748/wjg.v13.i16.2385 [Crossref] [ Google Scholar]
- Maeda Y, Shinohara T, Katayama T, Nagatsu A, Futakawa N, Hamada T. Gastrointestinal stromal tumor of the stomach with an abscess excised by laparoscopic surgery. Case Rep Gastroenterol 2016; 10(2):399-405. doi: 10.1159/000446578 [Crossref] [ Google Scholar]
- Ogino S, Kosuga T, Shoda K, Kubota T, Okamoto K, Otsuji E. Advanced gastric cancer with intramural abscess: a case report of a rare clinicopathological condition. In Vivo 2022; 36(4):1998-2001. doi: 10.21873/invivo.12925 [Crossref] [ Google Scholar]
- Smith GE. Subacute phlegmonous gastritis simulating intramural neoplasm: case report and review. Gastrointest Endosc 1972; 19(1):23-6. doi: 10.1016/s0016-5107(72)73938-3 [Crossref] [ Google Scholar]
- Will U, Masri R, Bosseckert H, Knopke A, Schönlebe J, Justus J. Gastric wall abscess, a rare endosonographic differential diagnosis of intramural tumors: successful endoscopic treatment. Endoscopy 1998; 30(4):432-5. doi: 10.1055/s-2007-1001297 [Crossref] [ Google Scholar]
- Nevin NC, Eakins D, Clarke SD, Carson DJ. Acute phlegmonous gastritis. Br J Surg 1969; 56(4):268-70. doi: 10.1002/bjs.1800560407 [Crossref] [ Google Scholar]
- Davies JP, Billings PJ, Jones MR. Intramural gastric abscess mimicking leiomyoma Clinical, radiologic, and pathologic features of an unusual gastric lesion. Invest Radiol 1993; 28(2):175-6. doi: 10.1097/00004424-199302000-00019 [Crossref] [ Google Scholar]
- Kiil C, Rosenberg J. Gastric intramural abscess successfully drained during gastroscopy. Gastrointest Endosc 2001; 53(2):231-2. doi: 10.1067/mge.2001.111559 [Crossref] [ Google Scholar]