Arch Iran Med. 26(2):117-118.
doi: 10.34172/aim.2023.18
Photoclinic
Cecal Volvulus: An Uncommon Diagnosis in a Child with Down’s Syndrome
Mohamed Zouari Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing, 1, 2, * 
Hana Ben Ameur Conceptualization, Data curation, Resources, Validation, 1, 2
Nesrine Ben Saad Resources, Validation, Writing – review & editing, 1, 2
Najoua Kraiem Data curation, Formal analysis, Investigation, 1, 2
Wiem Rhaiem Investigation, Visualization, 1, 2
Riadh Mhiri Supervision, 1, 2
Author information:
1Department of Pediatric Surgery, Hedi-Chaker Hospital, Sfax, Tunisia
2Research Laboratory “Developmental and Induced Diseases” (LR19ES12), Faculty of Medicine of Sfax, University of Sfax, Sfax, Tunisia
Copyright and License Information
© 2023 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Zouari M, Ben Ameur H, Ben Saad N, Kraiem N, Rhaiem W, Mhiri R. Cecal volvulus: An uncommon diagnosis in a child with down’s syndrome. Arch Iran Med. 2023;26(2):117-118. doi: 10.34172/aim.2023.18
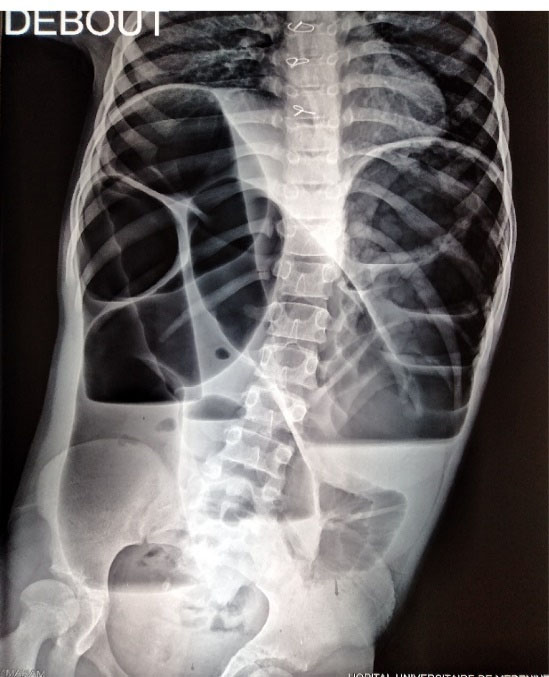
Figure 1.
Plain Abdominal X-ray Showing Large Dilated Loops of Colonic Bowel Occupying the Majority of Abdominal Cavity with Multiple Air-fluid Levels.
.
Plain Abdominal X-ray Showing Large Dilated Loops of Colonic Bowel Occupying the Majority of Abdominal Cavity with Multiple Air-fluid Levels.
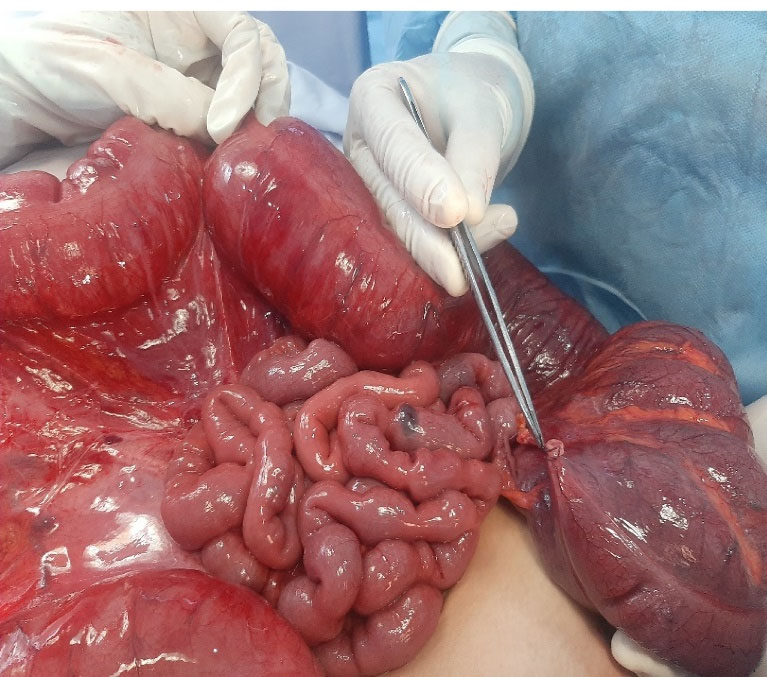
Figure 2.
Huge Dilated Colon. After Reduction of Cecal Volvulus, the Cecum and the Ascending Colon were Viable.
.
Huge Dilated Colon. After Reduction of Cecal Volvulus, the Cecum and the Ascending Colon were Viable.
A 12-year-old female child with mental retardation and Down’s syndrome presented to the emergency department for abdominal distension and bilious vomiting of a 3-day duration. No stool was passed in the last 24 hours. The patient had no history of abdominal surgery and no similar episodes. However, she had a long history of constipation.
Clinical examination revealed normal vital signs with a hugely distended tender abdomen. Rectal examination revealed stool but no blood. Radiography of the abdomen showed large dilated loops of colonic bowel occupying the majority of abdominal cavity with multiple air-fluid levels (Figure 1).
At laparotomy, we identified a 270-degree counter-clockwise volvulus involving the cecum and ascending colon. There was no fixation to the lateral retroperitoneum. There were no signs of intestinal ischemia (Figure 2). Therefore, we performed cecal detorsion, cecopexy and appendectomy. The postoperative course was complicated by an enterocutaneous fistula. This fistula was successfully managed by non-surgical treatment including sepsis control, optimization of nutritional status, and wound care. We discharged the patient on day thirty-two after surgery. The child was followed as an outpatient for 4 years, and currently has not experienced any recurrence.
Volvulus of the cecum is a diagnostic and therapeutic emergency. This condition, rare in adults, is extremely rare in children and accounts for less than 1% of acute intestinal obstructions in children.1,2 Several factors have been identified as risk factors for cecal volvulus, including malrotation, upward displacement of the cecum, colonic distension, and adhesions.2
Unless managed in a timely fashion, strangulation, resulting from the twisting of the intestine around its mesenteric axis, will lead to intestinal ischemia and ultimately to gangrene or bowel perforation. Therefore, intestinal resection is necessary in 19% to 50% of cecal volvulus cases.
Management of cecal volvulus is even more challenging in children with mental disability. These children commonly have aerophagia and constipation, which lead to bowel distension.3 The clinical presentation of cecal volvulus is usually non-specific. Therefore, a high suspicion level is essential to avoid diagnostic and therapeutic delays.4
Management of cecal volvulus is still controversial. Several publications have reported the safety and efficacy of conservative management based on detorsion with or without cecopexy in the absence of intestinal ischemia. However, most authors strongly recommend surgical cecal resection, as the gold standard to treat this condition.5-9
Competing Interests
All authors declare that they have no conflict of interest.
Ethical Approval
The patient and her parents gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Hedi-Chaker University Hospital (HCH-2022-1922).
References
- Rosenblat JM, Rozenblit AM, Wolf EL, DuBrow RA, Den EI, Levsky JM. Findings of cecal volvulus at CT. Radiology 2010; 256(1):169-75. doi: 10.1148/radiol.10092112 [Crossref] [ Google Scholar]
- Rakinic J. Colonic volvulus. In: Beck DE, Roberts PL, Saclarides TJ, Senagore AJ, Stamos MJ, Wexner SD, eds. The ASCRS Textbook of Colon and Rectal Surgery. New York, NY: Springer; 2011. p. 395-406. 10.1007/978-1-4419-1584-9_23.
- Takada K, Hamada Y, Sato M, Fujii Y, Teraguchi M, Kaneko K. Cecal volvulus in children with mental disability. Pediatr Surg Int 2007; 23(10):1011-4. doi: 10.1007/s00383-007-1987-6 [Crossref] [ Google Scholar]
- Solis Rojas C, Vidrio Duarte R, García Vivanco DM, Montalvo-Javé EE. Cecal volvulus: a rare cause of intestinal obstruction. Case Rep Gastroenterol 2020; 14(1):206-11. doi: 10.1159/000506933 [Crossref] [ Google Scholar]
- Mansoor K, Al Hamidi S, Khan AM, Samujh R. Rare case of pediatric cecal volvulus. J Indian Assoc Pediatr Surg 2009; 14(3):110-2. doi: 10.4103/0971-9261.57703 [Crossref] [ Google Scholar]
- Miura da Costa K, Saxena AK. A systematic review of the management and outcomes of cecal and appendiceal volvulus in children. Acta Paediatr 2018; 107(12):2054-8. doi: 10.1111/apa.14476 [Crossref] [ Google Scholar]
- Folaranmi SE, Cho A, Tareen F, Morabito A, Rakoczy G, Cserni T. Proximal large bowel volvulus in children: 6 new cases and review of the literature. J Pediatr Surg 2012; 47(8):1572-5. doi: 10.1016/j.jpedsurg.2011.10.064 [Crossref] [ Google Scholar]
- Madiba TE, Thomson SR. The management of cecal volvulus. Dis Colon Rectum 2002; 45(2):264-7. doi: 10.1007/s10350-004-6158-4 [Crossref] [ Google Scholar]
- van de Lagemaat M, Blink M, Bakx R, de Meij TG. Cecal volvulus in children: is there place for colonoscopic decompression?. J Pediatr Gastroenterol Nutr 2018; 66(2):e59-e60. doi: 10.1097/mpg.0000000000001766 [Crossref] [ Google Scholar]