Arch Iran Med. 25(3):194-195.
doi: 10.34172/aim.2022.33
Photoclinic
Paracoccidioidomycosis Simulating Eyelid Carcinoma
Juliano Peruzzo 1, *  , Luciana Cartelli Casagrande 1, Andre Silva Cartell 1, Marcelo Krieger Maestri 2, Fernando Procianoy 2, Perla Drescher de Castro Procianoy 1
, Luciana Cartelli Casagrande 1, Andre Silva Cartell 1, Marcelo Krieger Maestri 2, Fernando Procianoy 2, Perla Drescher de Castro Procianoy 1
Author information:
1Department of Dermatology, Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil
2Department of Ophtalmology, Hospital de Clínicas de Porto Alegre, Porto Alegre, RS, Brazil
*Corresponding Author: Juliano Peruzzo, MSc; 2350 Ramiro Barcelos St., Porto Alegre, Rio Grande do Sul, Brazil. Tel:+55-51- 33598571; Email:
julperuzzo@hcpa.edu.br
Copyright and License Information
© 2022 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Peruzzo J, Casagrande LC, Cartell AS, Maestri MK, Procianoy F, de Castro Procianoy PD. Photoclinic. Arch Iran Med. 2022;25(3):194-195. doi: 10.34172/aim.2022.33

Figure 1.
Vegetative and Exudative Lesion on the Right Upper Eyelid, with Erythema and Infiltration of the Upper and Lower Eyelids and Periocular Region.
.
Vegetative and Exudative Lesion on the Right Upper Eyelid, with Erythema and Infiltration of the Upper and Lower Eyelids and Periocular Region.
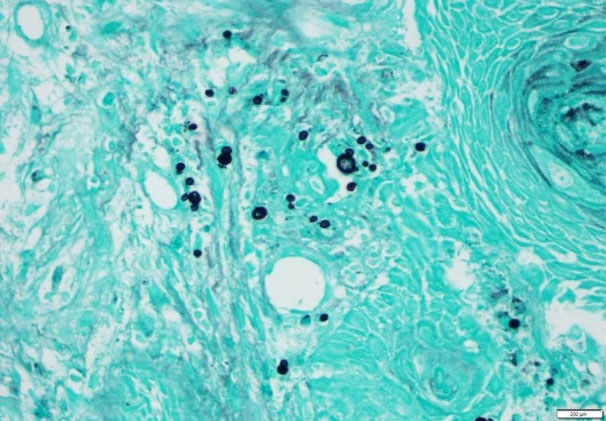
Figure 2.
Large Yeasts with More Than One Bud (Silver staining, 100X).
.
Large Yeasts with More Than One Bud (Silver staining, 100X).
A 60-year-old male, pottery worker, alcoholic and smoker patient presented to the Dermatology department due to a growing lesion in the right upper eyelid for about 6 months. He had already been treated with topical antibiotics without improvement. Upon examination, we observed an erythematous, vegetative and exudative plaque, with loss of right upper eyelid margin architecture and lower eyelid infiltration. Erythema and periocular infiltration were also observed (Figure 1).
Histopathologic study demonstrated presence of chronic suppurative inflammation associated with giant cells, epithelial pseudoepitheliomatous hyperplasia and suppurative foci. Silver staining showed large yeasts with more than one bud (Figure 2). A systemic investigation demonstrated lung involvement with moderate inflammatory infiltration on radiographs.
Paracoccidioidomycosis is caused by the thermodimorphic fungus Paracoccidioides brasiliensis. Its main route of transmission is by inhaling the spores and consequent hematogenous dissemination to other organs. However, contiguous lesions and direct inoculation can also occur.1-3 In the lung tissue, the fungus multiplies and the infectious focus may regress or remain latent for a period of up to 60 years, depending on the host’s cellular response. In individuals with a predominant Th1 response, it results in the formation of granulomas and control of fungal replication, although latent forms may remain viable. In patients with deficient Th1 response, there is no granuloma formation and an evolution to more severe clinical forms can occur.1,2,4 Gardening, soil preparation, and, mainly, agriculture are activities at greater risk of infection due to contact with contaminated soil.2,5
Paracoccidioidomycosis is divided into three different clinical forms: subclinical infection; disease, which comprise the acute/subacute (juvenile) and chronic (adult) forms; and the residual form (sequelae).1,2 The acute/subacute form mainly affects children and young adults and presents with rapid evolution and dissemination to the reticuloendothelial system, with involvement of multiple organs.Patients may present with lymphadenomegaly, hepatosplenomegaly, skin, mucous and osteoarticular lesions, gastrointestinal and, rarely, pulmonary involvement. The chronic form, on the other hand, represents 74%–96% of the cases, typically presents in adults and is more prevalent in males.2,4,6 Pulmonary involvement is present in 90% of these patients and oral mucosal and skin lesions are also frequent.2,5
Oculo-palpebral involvement is rare, occurs mainly due to hematogenous dissemination and can vary from madarosis to destructive ulcers indistinguishable from neoplasms.1,3,5 It usually presents as granulomatous ulcerated lesions with hemorrhagic fundus in the eyelids, and can affect the tear ducts, in addition to eyelid edema, hyperemia and infiltration.5
The gold standard for diagnosis is visualization of the fungus by direct examination, specific stains such as periodic acid-Schiff (PAS) and Grocott on histopathological exam, or even by culture.1,3,4 The presence of multiple buds in a “ship’s wheel” appearance is pathognomonic.3
Treatment is based on the severity of the disease. For mild or moderate forms, itraconazole is the first choice; other options are sulfamethoxazole-trimethoprim and voriconazole. For severe cases, intravenous amphotericin B is recommended.1,2,6 Our patient was treated with 200 mg itraconazole per day, with a significant improvement in the first month (Figure 3).
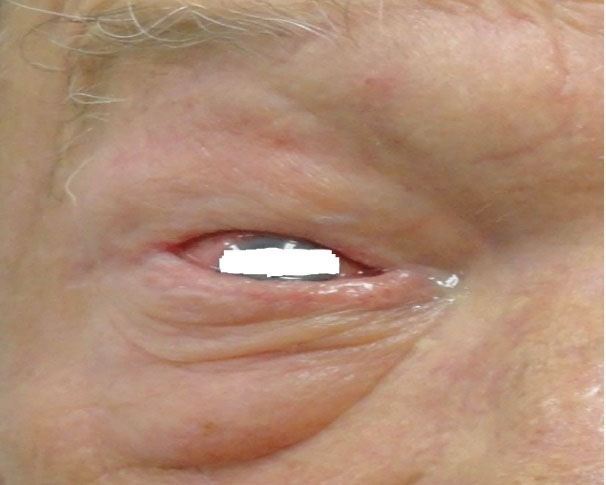
Figure 3.
Improvement of Lesions in the Right Eyelid after Treatment, Remaining Only with Conjunctival Hyperemia and Mild Periocular Erythema.
.
Improvement of Lesions in the Right Eyelid after Treatment, Remaining Only with Conjunctival Hyperemia and Mild Periocular Erythema.
Authors’ Contribution
All authors have been involved in the patient case. The manuscript was written especially by LCC and JP and the other authors were responsible for its review.
Conflict of Interest Disclosures
The authors declare they have no conflict of interest.
Ethical Statement
The patient consented with the photographs and the case is in accordance with our institution protocols.
References
- Marques SA. Paracoccidioidomycosis. Clin Dermatol 2012; 30(6):610-5. doi: 10.1016/j.clindermatol.2012.01.006 [Crossref] [ Google Scholar]
- Shikanai-Yasuda MA, Mendes RP, Colombo AL, Queiroz-Telles F, Kono ASG, Paniago AMM. Brazilian guidelines for the clinical management of paracoccidioidomycosis. Rev Soc Bras Med Trop 2017; 50(5):715-40. doi: 10.1590/0037-8682-0230-2017 [Crossref] [ Google Scholar]
- Odashiro AN, Odashiro PR, Fernandes PI, Leite LV, Odashiro M, Maloney S. Eyelid and conjunctival paracoccidioidomycosis simulating carcinoma. Int Ophthalmol 2011; 31(1):63-7. doi: 10.1007/s10792-010-9407-7 [Crossref] [ Google Scholar]
- Cruz AA, Zenha F, Silva JT Jr, Martinez R. Eyelid involvement in paracoccidioidomycosis. Ophthalmic Plast Reconstr Surg 2004; 20(3):212-6. doi: 10.1097/01.iop.0000123499.39109.1d [Crossref] [ Google Scholar]
- de Oliveira Rassi TN, Passos RR, Kumagai KM, Soranz Filho JE, Holanda de Freitas JA. [Chronical and multifocal paracoccidioidomycosis having the lid involvement as the first sign: case report]. Arq Bras Oftalmol 2009; 72(6):822-5. doi: 10.1590/s0004-27492009000600016 [Crossref] [ Google Scholar]
- Shikanai-Yasuda MA. Paracoccidioidomycosis treatment. Rev Inst Med Trop Sao Paulo 2015; 57 Suppl 19(Suppl 19):31-7. doi: 10.1590/s0036-46652015000700007 [Crossref] [ Google Scholar]