Arch Iran Med. 25(3):191-193.
doi: 10.34172/aim.2022.32
Case Report
Adenoid Cystic Carcinoma with Intracranial Extension
Masoud Asghari 1  , Mahdieh Rajabi-Moghaddam 2, Hamid Abbaszadeh 3, *
, Mahdieh Rajabi-Moghaddam 2, Hamid Abbaszadeh 3, * 
Author information:
1Department of Otorhinolaryngology, School of Medicine, Birjand University of Medical Sciences, Birjand, Iran
2Department of Pathology, School of Medicine, Birjand University of Medical Sciences, Birjand, Iran
3Department of Oral and Maxillofacial Pathology, School of Dentistry, Birjand University of Medical Sciences, Birjand, Iran
*Corresponding Author: Hamid Abbaszadeh, DDS; Oral and Maxillofacial Pathology Department, Faculty of Dentistry, Birjand, South Khorasan Province, Iran. Tel:+98-915-8002580; Fax:+98-56-32381700; Email:
hamidabbaszade@yahoo.com
Abstract
Adenoid cystic carcinoma (ADCC) is a malignant tumor of salivary gland origin. ADCC of sinonasal tract is rare. We present a rare and unresectable case of sinonasal ADCC with intracranial extension in an 83-year-old man with the chief complaint of nasal congestion. Invasion to the maxillary sinus, nasopharynx, anterior cranial fossa, sella turcica and extension to cavernous sinus, dura mater and infratemporal fossa were evident on MRI and CT scan. The patient was treated only by palliative radiotherapy, but unfortunately, he died 3 months after the initial diagnosis.
Keywords: Adenoid cystic carcinoma, Nose neoplasms, Paranasal sinuses, Skull
Copyright and License Information
© 2022 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Asghari M, Rajabi-Moghaddam M, Abbaszadeh H. Adenoid cystic carcinoma with intracranial extension. Arch Iran Med. 2022;25(3):191-193. doi: 10.34172/aim.2022.32
Introduction
Adenoid cystic carcinoma (ADCC) is a rare malignant tumor of salivary gland origin.1,2 Five to ten percent of salivary gland tumors are ADCC and this tumor consists < 1% of head and neck malignancies.1,3 The occurrence of malignancy in sinonasal tract is infrequent.4 Sinonasal cancers account for approximately 4% of all head and neck malignancies. ADCC account for 5% of all sinonasal malignancies.5 ADCC originates from the minor mucosal glands of the nasal epithelium or paranasal sinuses epithelium. ADCC occurs predominantly in 40- to 60-year-old females.6 Some symptoms of sinonasal ADCCs are similar to symptoms of chronic sinusitis; therefore, the diagnosis of sinonasal ADCC is often delayed.7 It is characterized by slow growth, local invasion and perineural spreading. Due to local aggressiveness and slow growth, patients can present with huge and unresectable tumors.1 ADCCs with extension beyond the base of the skull have been rarely reported. ADCCs show high rates of locoregional recurrence and rare regional lymph node metastases. Distant metastasis usually occurs long after the initial diagnosis of ADCC and is more frequent than regional lymph node metastasis, with metastatic disease occurring in the lung and bone.2,5
Case Report
It should be noted that written consent was obtained from the patient we are reporting. The patient was an 83-year-old man who complained of obstruction and nasal congestion of two months’ duration and referred to the otorhinolaryngology department of Razi Hospital in Birjand, South Khorasan Province, Iran. On initial examination, proptosis of the right eye was observed with ptosis of the right eyelid. Past medical history was not remarkable. The physical exam of the nose showed a bulging mass of the right nasal cavity that filled the cavity along with involvement of the nasal septum. Neck examination was normal for lymph nodes. A cranial CT scan showed a lesion with involvement of the sella turcica and lateral wall of the sphenoid sinus, which entered the cavernous sinus, extended to dura mater and involved the infratemporal fossa. MRI of the patient showed a large enhancing soft tissue nasal cavity lesion which had destroyed the septum and invaded the right maxillary sinus, nasopharynx, and the anterior cranial fossa with involvement of the sella turcica. Turbidity was seen in the paranasal and mastoid sinuses on both sides. Atrophy of the brain parenchyma with foci of deep white matter hyperintensities on both sides (indicating chronic microvascular changes) was evident (Figure 1). Chest and abdominal CT scans showed no distant metastasis. Clinical stage IVB (T4bN0M0) was assigned to the tumor. The following differential diagnoses were proposed: (1) Nasopharyngeal carcinoma; (2) Squamous cell carcinoma; and (3) ADCC. The patient underwent an incisional biopsy of the sinonasal mass. Histopathologic examination showed sinonasal tissue infiltrated by neoplastic lesion with solid and tubular pattern. There were sheets of hyperchromatic monotonous basaloid cells (Figure 2). Histopathologic findings were suggestive of the following differential diagnoses: (1) ADCC; (2) polymorphous low-grade adenocarcinoma (PLGA); and 3) metastatic breast carcinoma. Additional immunohistochemical markers showed positive immunostaining for CD117 (C-kit) (strong and diffuse staining), SMA, P-63, S-100, vimentin, and CK7, and negative immunostaining for GCDF-15. Finally, the lesion was diagnosed as ADCC (grade II according to van Weert grading system). Because the tumor was unresectable (due to tumor extension), the patient was referred to a radiation oncologist for palliative radiotherapy and primary tumor control. The radiation oncologist made a volumetric arc therapy treatment plan with the goal of 70 Gy to the tumor. Unfortunately, after 10 courses of radiation therapy which was three months after the initial diagnosis, the patient died due to the tumor invading vital structures in the brain.
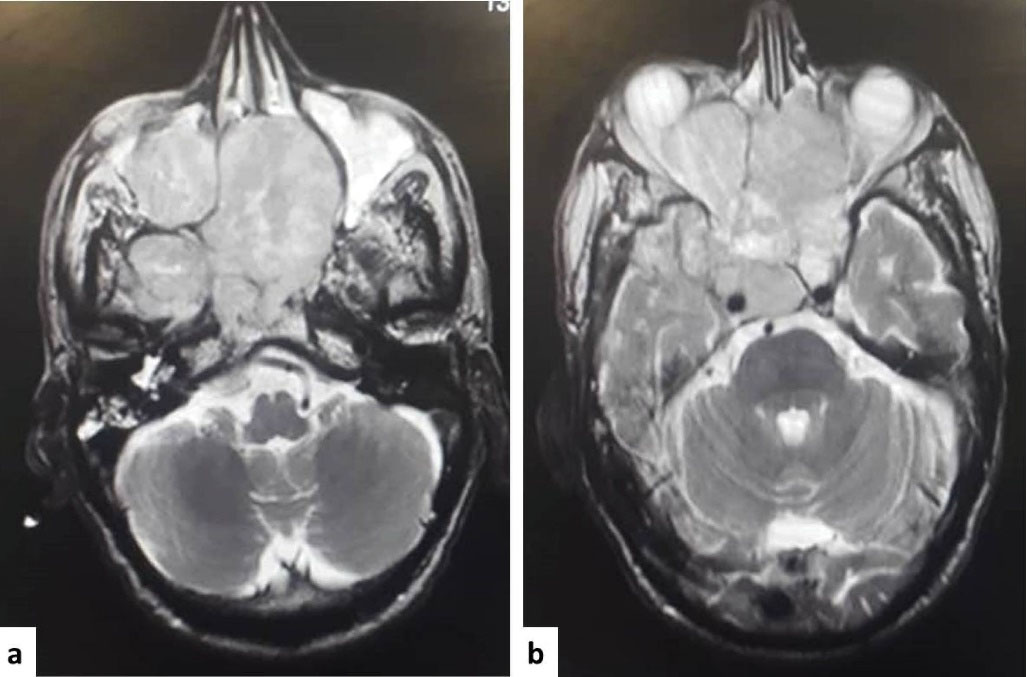
Figure 1.
MRI showing (a) a large enhancing soft tissue lesion in the nasal cavity along with destruction of the septum of the nose and invasion to the right maxillary sinus, nasopharynx; (b) involvement of the anterior cranial fossa, sella turcica and cavernous sinus.
.
MRI showing (a) a large enhancing soft tissue lesion in the nasal cavity along with destruction of the septum of the nose and invasion to the right maxillary sinus, nasopharynx; (b) involvement of the anterior cranial fossa, sella turcica and cavernous sinus.
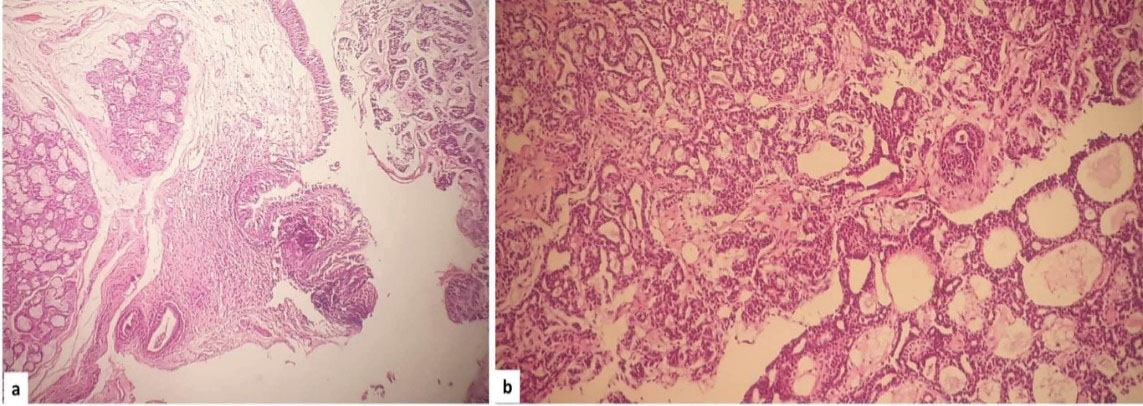
Figure 2.
Histopathologic view showing (a) sections of tumor tissue beneath the respiratory nasal epithelium (Hematoxylin & Eosin, 40X); (b) sheets of hyperchromatic monotonous basaloid cells with solid and tubular pattern (Hematoxylin & Eosin, 100X).
.
Histopathologic view showing (a) sections of tumor tissue beneath the respiratory nasal epithelium (Hematoxylin & Eosin, 40X); (b) sheets of hyperchromatic monotonous basaloid cells with solid and tubular pattern (Hematoxylin & Eosin, 100X).
Discussion
Annually, 3 to 4.5 cases of ADCC occur in every one million people. Perineural invasion (PNI) is a characteristic feature of ADCC; this feature can help the tumor to spread to the base of the skull.2
The imaging features of ADCCs consist of irregular lesions along with destruction of the bone and heterogeneous density or high-signal-intensity. PNI is best recognized by MRI; in this regard, it is better than CT.6
In a case series by Volpi et al, the ethmoid sinus was the primary tumor site for most of sinonasal ADCCs.5 In our case, the primary tumor site was probably the nasal cavity. In their case series, most sinonasal ADCCs presented at T3 or T4 (given the tumor size) without any systemic spreading. Our case presented at T4b without any metastasis. They reported transnasal endoscopic craniectomy for ADCC with spreading to base of the skull. In our case, the patient did not undergo surgical resection and the only management was radiotherapy. In their case series, the five-year overall survival rate was 86.5%. They concluded that greater tumor size, higher grading (grade III), involved margin and PNI contribute to poor prognosis. Jang et al reported that older age, skull base involvement, and metastatic disease predicted a worse overall survival for ADCC of the head and neck region.8
Hajar et al reported a case of nasopharyngeal ADCC with intracranial extension in a 20-year-old patient.1 Intracranial extension was a common feature in our case and theirs. Histological evaluation revealed cribriform and tubular patterns. In our case, solid and tubular patterns prevailed.
Giridhar et al presented an ADCC in sphenoid sinus which invaded the internal structures of the cranium; it occurred in a 38-year-old man and was treated successfully with radical radiation at 6-month follow-up.4 Sepúlveda et al presented a 51-year-old patient with sinonasal ADCC in the right nasal cavity with spreading to the middle part of the cranium; the patient was treated by radiochemotherapy. Follow-up was not mentioned.6
The three histologic patterns of ADCC are solid, tubular and cribriform. These patterns are related to prognosis; the solid pattern has been associated with the worst prognosis.5 Treatment of ADCCs associated with the involvement of the base of skull is problematic; they may be difficult to resect.9 There is no agreement on the treatment of these ADCCs and different surgeons and therapeutic teams may treat these tumors in different manners.10 When the tumor is resectable, surgical resection with or without radiotherapy is the treatment of choice. In advanced tumors that are unresectable, radiotherapy is the only therapeutic option. New conformational radiotherapies such as IMRT (Intensity Modulated Radiation Therapy), tomotherapy and arc therapy are among radiotherapy techniques. Photons therapy, neutrons therapy, protons therapy and carbon ions are other treatment paradigms.1 Xu et al reported 125I brachytherapy to be a good management option for the above-mentioned ADCCs.9
Guazzo and Panizza demonstrated that survival is favorable in ADCCs spreading to base of the skull.2 In their study, although overall survival appeared favorable in these ADCCs, a great amount of metastasis was shown. Contrary to their claims, Volpi et al stated that in sinonasal ADCC, survival over a wide period of time is poor; the patients often die of regional recurrence, not from metastasis. Due to proximity to vital structures, proximity to nerves, and late diagnosis, complete tumor resection with tumor-free margins is difficult.5
To conclude, the similarity of the symptoms of sinonasal ADCCs to those of chronic sinusitis, along with the slow growth and perineural propensity of ADCC, can delay the diagnosis and result in intracranial extension which in turn complicates the treatment plan; in such cases, management should be made in a multidisciplinary specialized center with consultation in a tumor board to select the best treatment option.
Authors’ Contribution
MA, MRM, HA: Study concept and design, data acquisition and drafting of manuscript, and critical revision of the manuscript.
Conflict of Interest Disclosures
All authors declare that they have no conflict of interest.
Ethical Statement
This study was approved by ethical committee of Birjand University of Medical Sciences (ethic code: IR.BUMS.REC.1399.545). Informed consent was obtained from the patient.
References
- Hajar TS, Seka E, Aarab J, Omor Y, Elkacemi H, Elmajjaoui S. An unusual case of nasopharyngial adenoid cystic carcinoma with intracranial and orbital extension: a challenge for innovative conformal radiotherapy techniques. Ann Clin Med Case Rep 2020; 4(2):1-3. doi: 10.15761/crr.1000206 [Crossref] [ Google Scholar]
- Guazzo E, Panizza B. Management of advanced adenoid cystic carcinoma infiltrating the skull base: a contemporary review. J Neurooncol 2020; 150(3):419-27. doi: 10.1007/s11060-019-03366-x [Crossref] [ Google Scholar]
- Gentile MS, Yip D, Liebsch NJ, Adams JA, Busse PM, Chan AW. Definitive proton beam therapy for adenoid cystic carcinoma of the nasopharynx involving the base of skull. Oral Oncol 2017; 65:38-44. doi: 10.1016/j.oraloncology.2016.11.016 [Crossref] [ Google Scholar]
- Giridhar P, Mallick S, Laviraj MA, Bhasker S. Adenoid cystic carcinoma sphenoid sinus with intracranial extension treated by radical radiotherapy: a rare case. Eur Arch Otorhinolaryngol 2015; 272(4):1037-40. doi: 10.1007/s00405-014-3441-4 [Crossref] [ Google Scholar]
- Volpi L, Bignami M, Lepera D, Karligkiotis A, Pistochini A, Ottini G. Endoscopic endonasal resection of adenoid cystic carcinoma of the sinonasal tract and skull base. Laryngoscope 2019; 129(5):1071-7. doi: 10.1002/lary.27485 [Crossref] [ Google Scholar]
- Sepúlveda I, Platin E, Delgado C, Rojas P. Sinonasal adenoid cystic carcinoma with intracranial invasion and perineural spread: a case report and review of the literature. J Clin Imaging Sci 2015; 5:57. doi: 10.4103/2156-7514.168710 [Crossref] [ Google Scholar]
- Lee YC, Lee TJ, Tsang NM, Huang Y, Hsu CL, Hsin LJ. Cavernous sinus involvement is not a risk factor for the primary tumor site treatment outcome of sinonasal adenoid cystic carcinoma. J Otolaryngol Head Neck Surg 2018; 47(1):12. doi: 10.1186/s40463-018-0257-z [Crossref] [ Google Scholar]
- Jang S, Patel PN, Kimple RJ, McCulloch TM. Clinical outcomes and prognostic factors of adenoid cystic carcinoma of the head and neck. Anticancer Res 2017; 37(6):3045-52. doi: 10.21873/anticanres.11659 [Crossref] [ Google Scholar]
- Xu N, Zheng L, Wu WJ, Huang MW, Zhang J, Zhang JG. Definitive 125I brachytherapy of locally advanced adenoid cystic carcinoma involving the skull base with satisfying efficacy and safety. J Oral Maxillofac Surg 2019; 77(10):2143-53. doi: 10.1016/j.joms.2019.03.031 [Crossref] [ Google Scholar]
- Guazzo E, Bowman J, Porceddu S, Webb L, Panizza B. Advanced adenoid cystic carcinoma of the skull base - the role of surgery. Oral Oncol 2019; 99:104466. doi: 10.1016/j.oraloncology.2019.104466 [Crossref] [ Google Scholar]