Arch Iran Med. 25(6):360-365.
doi: 10.34172/aim.2022.59
Original Article
Incidence, Time Trends and Geographical Distribution of Leukemia and Multiple Myeloma in Golestan Province, Northern Iran, 2004–2017
Nastaran Jafari-Delouei 1  , Mohammad Naimi-Tabiei 2
, Mohammad Naimi-Tabiei 2  , Mehran Farajollahi 1
, Mehran Farajollahi 1  , Seyed Mehdi Sedaghat 3
, Seyed Mehdi Sedaghat 3  , Seyyedreza Khandoozi 2
, Seyyedreza Khandoozi 2  , Fatemeh Ghasemi-Kebria 1
, Fatemeh Ghasemi-Kebria 1  , Roshan Dinparastisaleh 4
, Roshan Dinparastisaleh 4  , Amirhoushang Pourkhani 2, *
, Amirhoushang Pourkhani 2, *  , Gholamreza Roshandel 1, *
, Gholamreza Roshandel 1, * 
Author information:
1Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran
2Cancer Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3Deputy of Public Health, Golestan University of Medical Sciences, Gorgan, Iran
4Outcomes After Critical Illness and Surgery Group, Johns Hopkins University, Division of Pulmonary and Critical Care Medicine, Johns Hopkins School of Medicine, Baltimore, MD, USA
*
Corresponding Authors: Gholamreza Roshandel, MD; Golestan Research Center of Gastroenterology and Hepatology, Sayyad Shirazi hospital, Gorgan, Iran. Tel: + 98 911 375 7327, Email:
roshandel_md@yahoo.com; Amirhoushang Pourkhani, MD; Cancer Research Center, Sayyad Shirazi Hospital, Sayyad Shirazi Bulevard, Gorgan, Iran. Tel: + 98 32251910, Email:
dr.amir.h.pourkhani@gmail.com
Abstract
Background:
Leukemia and multiple myeloma (MM) are the most common hematologic malignancies in Iran. This paper describes the geographic and temporal changes in their incidence in Golestan, northern Iran.
Methods:
Data on cases of leukemia and MM during 2004–2017 were obtained from the Golestan Population-based Cancer Registry (GPCR). The GPCR is a dynamic database of Golestan residents diagnosed with primary cancers. Age-standardized incidence rates (ASRs) (per 100000) of leukemia and MM were calculated using direct standardization method considering the world standard population. We used Joinpoint regression to assess incidence trends using the average annual percent change (AAPC).
Results:
In total, 2119 new cases of leukemia and MM were registered by the GPCR during 2004–2017. The ASRs of leukemia were 9.71 and 6.70 in males and females, respectively, while the rates were lower for MM: 2.66 and 1.97 in males and females, respectively. The incidence rates of leukemia suggested an increasing trend in urban population (AAPC=2.73; P value=0.154), while in rural area, the incidence rates were slightly decreasing (AAPC=- 0.73; P value=0.658). There were high incidence areas of leukemia in the central and western regions of Golestan.
Conclusion:
Our results suggested high incidence rates of leukemia and MM in the Golestan province. We also found geographical diversities and increasing trends in the incidence of leukemia in the urban population. Exposure to occupational and environmental carcinogens including pesticides may partly explain high rates and the observed trends. Further investigations should be considered to clarify these points in our population.
Keywords: Epidemiology, Golestan, Iran, Leukemia, Multiple myeloma
Copyright and License Information
© 2022 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Jafari-Delouei N, Naimi-Tabiei M, Farajollahi M, Sedaghat SM, Khandoozi S, Ghasemi-Kebria F, et al. Incidence, time trends and geographical distribution of leukemia and multiple myeloma in golestan province, Northern Iran, 2004–2017. Arch Iran Med. 2022;25(6):360-365. doi: 10.34172/aim.2022.59
Introduction
Cancer, previously the leading cause of death in most of the developed countries will be a major cause of morbidity and death in the near future in different part of the world, irrespective of the status of resources.1 Cancer is the leading cause of mortality in high-income countries and the second cause of mortality in the developing world.2 Hematologic malignancies comprise a collection of heterogeneous diseases characterized by the uncontrolled growth of hematopoietic cells. Different factors have been proposed to play a role in the development of hematologic malignancies including infectious diseases (e.g., HTLV-1 and adult T-cell leukemia/lymphoma), autoimmune disorders (e.g., rheumatoid arthritis, systemic lupus erythematous and Sjogren syndrome) or positive family history.3
Hematologic malignancies include different disorders some of which are progressive, malignancies of the blood-forming organs, characterized by distorted proliferation and development of leukocytes and their precursors in the blood and bone marrow, and others are due to lymphatic tissue involvement.4 The three major types of hematologic malignancies are leukemia, lymphoma, and plasma cell disorders.5 Leukemia is a malignant proliferation of hematopoietic cells in the bone marrow followed by dissemination into the blood and infiltration into soft tissue.6 Extramedullary manifestations may occur in different organs (e.g. skin), following a generalization phase in the bone marrow and the subsequent dissemination of cancer cells in the peripheral blood.6 Leukemia may be classified based on the its biological behavior and the immunophenotypical, morphological, and cytogenetic characteristics of neoplastic cells in chronic and acute, myeloid or lymphocytic forms of disease.7,8 Acute leukemia has been classified by the French‐American‐British (FAB) Cooperative Group. The FAB classification of acute lymphocytic leukemia includes three subtypes (L1–L3), while acute myeloid leukemia is divided into 8 subtypes (M0–M7).9 Multiple myeloma (MM) is the second most common hematologic malignancy. It is described in the spectrum of plasma cell dyscrasias, ranging from monoclonal gammopathy of unknown significance to overt plasma cell leukemia and extramedullary myeloma. MM may result in significant morbidity due to its effects on end-organ damage and older population involvement.10 After decades of virtually no improvement, the MM survival rate has seen major progress in the last 10 years, even 2- to 3-fold in younger patients.11 According to GLOBOCAN 2018 estimates of global cancer incidence, leukemia and MM with 437.033 and 159.985 new cases per year, respectively, are amongst the commonly diagnosed malignancies in the world.12 The age-standardized incidence rates (ASRs) of leukemia and MM are higher among males, but in North America, Australia, New Zealand and Europe, the male preponderance may be even more remarkable.12 Leukemia ranked 7th among the most commonly diagnosed cancers in Iran with 2,174 new cases per year (4.3% of all cases) and a higher ASR in males (8.6 per 100 000) versus females (5.9 per 100 000).12
Golestan is one of the 31 provinces, located in Northern Iran. As a voting member of the International Association of Cancer Registries (IACR), the Golestan Population-based Cancer Registry (GPCR), has been providing high-quality reports on Golestan cancer statistics, since 2004. Previous GPCR reports revealed higher rates of leukemia in the Golestan province, compared with other provinces.13 In this paper, we aimed to present an updated report on incidence rates and epidemiology trends of leukemia and MM in the Golestan province of Iran.
Materials and Methods
This study was conducted on primary incidence data of leukemia and MM in Golestan, Northern Iran. Golestan is one of the 31 provinces of Iran with about 1.9 million population in 2016 (2.3% of total population of Iran) and an area of about 20 000 km.2
The GPCR, a population-based cancer registry, covers the total population of the Golestan province. The GPCR is a dynamic database of Golestan and territory residents, who were diagnosed with primary cancers (alive or dead). The GPCR database provides demographic, geographic, and clinical information, including the patient’s gender, diagnosis year, age at diagnosis, and residence place as well as the tumor characteristics. Data of the GPCR were collected from all the private and public healthcare centers throughout the Golestan province,and the deputy of health of the Golestan University of Medical Science (GOUMS) sends regular updates on cancer-related deaths.14 Additionally, we collected data from sources outside of Golestan to minimize underestimation of new cases due to potential referral to neighboring provinces (e.g. Khorasan Razavi and Tehran).We used the third version of the International Classification of Diseases for Oncology (ICD-O-3) system for coding tumor characteristics.15
For this study, we examined the data on the incidence of leukemia and MM in the GPCR between 2004 and 2017. We used the CanReg-5 software16,17 to calculate the age-specific rates, crude rates and the ASRs.18 ASRs were calculated by direct standardization method using the 18 age groups world standard population. All rates were presented per 100 000 person-years. Joinpoint regression analysis was used to assess time trends during the study period19 using the average annual percent change (AAPC) and its corresponding 95% confidence intervals (CIs).
Results
During the study period (2004-2017), a total of 2119 new cases of leukemia and MM were registered in the GPCR with a mean (SD) age of 46.8 (23.9) years, at diagnosis. Of these, 1697 were diagnosed with leukemia with a mean (SD) age of 43.5 (24.7) years, and 422 were diagnosed with MM with a mean (SD) age of 60.1 (13.7) years.
The number (crude rate; ASR) of leukemia cases were 993 (8.16; 9.71) and 704 (5.77; 6.70) per 100 000 person-year in males and females, respectively. The number (crude rate; ASR) of MM cases were 238 (1.96; 2.66) and 184 (1.51; 1.97) per 100 000 person-year in males and females, respectively (Table 1). Table 2 shows the number, crude rate, ASR and 95% CI of ASR for leukemia in Golestan by incidence year and sex. The number, crude rate, ASR, and 95% CI of ASR for MM and different types of leukemia in the Golestan province by incidence, year, and gender are shown in Table S1 (see Supplementary file 1). Figure 1 shows the age-specific incidence rates of leukemia by gender. As shown in Figure 1, the leukemia incidence rate peaks at the age group 75-79 and 80-84 in males and females, respectively.
Table 1.
Number, Crude Rate and ASR and 95% Confidence Interval (Per 100 000 Person-Year) of Leukemia and Multiple Myeloma by Morphology and Gender in Golestan, Iran during 2004 to 2017
|
|
Male
|
Female
|
All
|
|
Number
|
Crude
|
ASR
|
ASR-L
|
ASR-U
|
Number
|
Crude
|
ASR
|
ASR-L
|
ASR-U
|
Number
|
Crude
|
ASR
|
ASR-L
|
ASR-U
|
| Lymphoid-leukemia |
436 |
3.58 |
4.34 |
3.91 |
4.77 |
246 |
2.02 |
2.43 |
2.12 |
2.74 |
682 |
2.8 |
3.38 |
3.13 |
3.63 |
| Myeloid-leukemia |
274 |
2.25 |
2.6 |
2.29 |
2.91 |
224 |
1.84 |
2.11 |
1.82 |
2.4 |
498 |
2.04 |
2.35 |
2.13 |
2.57 |
| Unspecified-leukemia |
283 |
2.33 |
2.78 |
2.45 |
3.11 |
234 |
1.92 |
2.16 |
1.87 |
2.45 |
517 |
2.12 |
2.46 |
2.24 |
2.68 |
| MM |
238 |
1.96 |
2.66 |
2.31 |
3.01 |
184 |
1.51 |
1.97 |
1.68 |
2.26 |
422 |
1.73 |
2.31 |
2.07 |
2.55 |
ASR, Age-standardized incidence rate; ASR-L, Lower limit of 95% CI; ASR-U, Upper limit of 95% CI; MM, multiple myeloma.
Table 2.
Number, Crude Rate and ASR and 95% Confidence Interval (Per 100 000 Person-Year) of Leukemia by Incidence Year and Gender in Golestan, Iran, 2004–2017
|
Year
|
Male
|
Female
|
|
Number
|
Crude
|
ASR
|
ASR-L
|
ASR-U
|
Number
|
Crude
|
ASR
|
ASR-L
|
ASR-U
|
| 2004 |
48 |
6.22 |
7.84 |
5.47 |
10.21 |
26 |
3.32 |
4.14 |
2.45 |
5.83 |
| 2005 |
72 |
9.14 |
10.91 |
8.24 |
13.58 |
43 |
5.39 |
6.90 |
4.69 |
9.11 |
| 2006 |
64 |
7.96 |
11.1 |
8.2 |
14.00 |
51 |
6.27 |
7.80 |
5.53 |
10.07 |
| 2007 |
73 |
8.90 |
10.26 |
7.79 |
12.73 |
50 |
6.04 |
7.68 |
5.45 |
9.91 |
| 2008 |
73 |
8.72 |
10.91 |
8.26 |
13.56 |
56 |
6.64 |
7.64 |
5.50 |
9.78 |
| 2009 |
62 |
7.27 |
8.22 |
6.04 |
10.40 |
52 |
6.06 |
7.75 |
5.57 |
9.93 |
| 2010 |
69 |
7.94 |
9.77 |
7.34 |
12.20 |
46 |
5.26 |
6.11 |
4.29 |
7.93 |
| 2011 |
59 |
6.66 |
7.57 |
5.55 |
9.59 |
25 |
2.81 |
3.29 |
1.94 |
4.64 |
| 2012 |
62 |
6.92 |
7.75 |
5.73 |
9.77 |
43 |
4.79 |
5.47 |
3.78 |
7.16 |
| 2013 |
52 |
5.73 |
6.66 |
4.76 |
8.56 |
48 |
5.30 |
5.34 |
3.79 |
6.89 |
| 2014 |
66 |
7.19 |
8.69 |
6.51 |
10.87 |
49 |
5.36 |
5.99 |
4.27 |
7.71 |
| 2015 |
96 |
10.35 |
11.43 |
9.1 |
13.76 |
79 |
8.57 |
9.60 |
7.42 |
11.78 |
| 2016 |
101 |
10.76 |
12.17 |
9.7 |
14.64 |
78 |
8.38 |
8.86 |
6.82 |
10.90 |
| 2017 |
96 |
10.12 |
11.55 |
9.16 |
13.94 |
58 |
6.18 |
6.72 |
4.94 |
8.50 |
ASR, Age-standardized incidence rate; ASR-L, Lower limit of 95% CI; ASR-U, Upper limit of 95% CI.
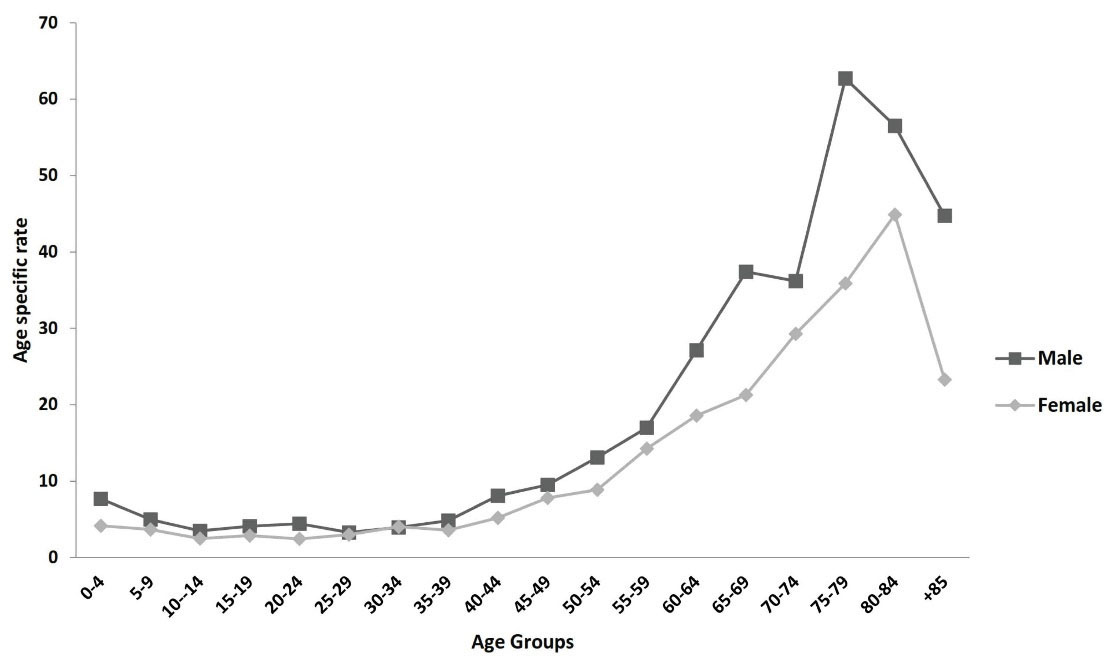
Figure 1.
Age Specific Incidence Rate (Per 100 000 Person-Year) of Leukemia in Golestan, Iran, during 2004–2017.
.
Age Specific Incidence Rate (Per 100 000 Person-Year) of Leukemia in Golestan, Iran, during 2004–2017.
Figure 2 shows the temporal trends of leukemia over the last decade, suggesting no significant trends in both males (AAPC = 0.54; 95% CI: - 2.33 to 3.49; P value = 0.693) and females (AAPC = 1.27; 95% CI: -3.03 to 5.75; P value = 0.539), whereas the changes were more considerable in females.
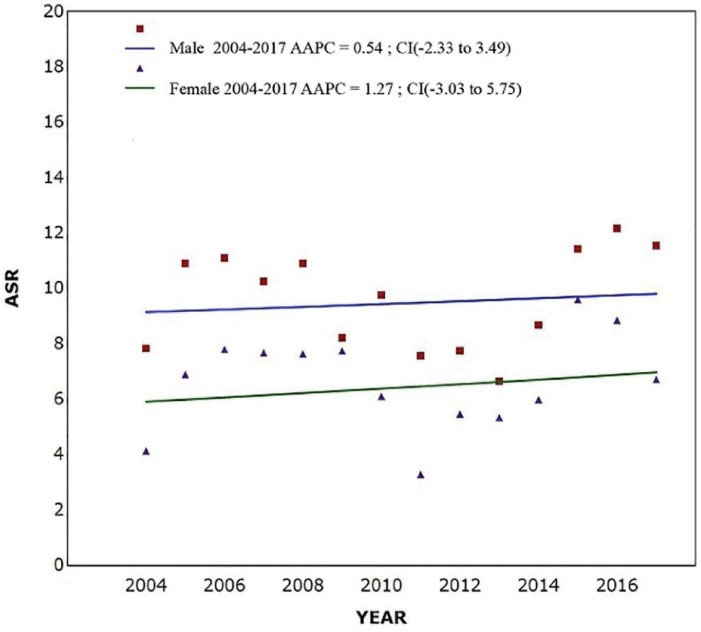
Figure 2.
Temporal Variations in Age Standardized Incidence Rate of Leukemia in Golestan, Iran, by Sex, during 2004-2017. AAPC, Average annual percent changes; CI, confidence interval; ACR, age standardized incidence rate.
.
Temporal Variations in Age Standardized Incidence Rate of Leukemia in Golestan, Iran, by Sex, during 2004-2017. AAPC, Average annual percent changes; CI, confidence interval; ACR, age standardized incidence rate.
The number (crude rate; ASR) of leukemia cases were 843 (6.78; 8.07) and 845 (7.16; 8.37) per 100 000 person-year in urban and rural regions, respectively. Figure 3 shows the time trends of incidence of leukemia in urban and rural areas of the Golestan province. The findings suggested an increasing trend in the urban population (AAPC = 2.73; 95% CI: -1.16 to 6.78; P value = 0.154), while in the rural area, the incidence rates were slightly decreasing (AAPC = -0.73; 95% CI: -4.15 to 2.82; P value = 0.658). Figure 4 demonstrates the geographical distribution of leukemia in subdivisions of the Golestan province by gender. The incidence rates of leukemia were highest in central and western parts of the province.
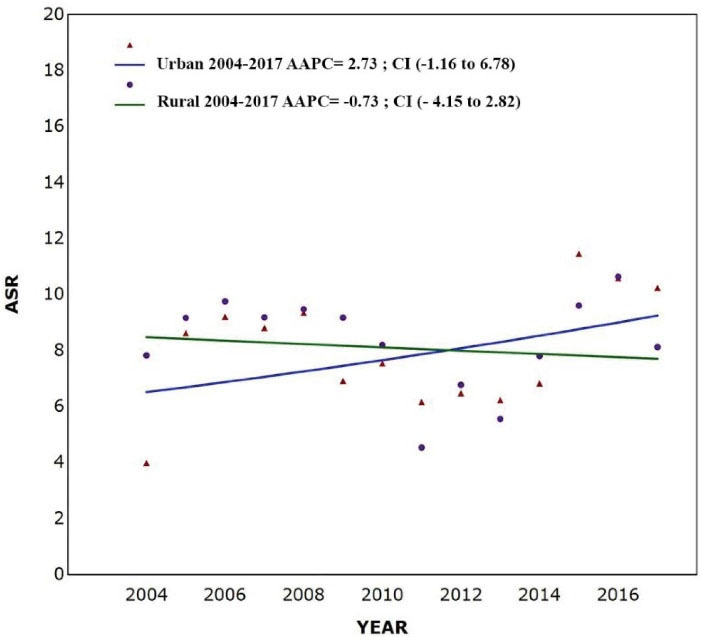
Figure 3.
Time trends in Age Standardized Incidence Rate of Leukemia in Golestan, Iran, by Residence Area, during 2004–2017. AAPC, Average annual percent changes; CI, confidence interval; ACR, age standardized incidence rate.
.
Time trends in Age Standardized Incidence Rate of Leukemia in Golestan, Iran, by Residence Area, during 2004–2017. AAPC, Average annual percent changes; CI, confidence interval; ACR, age standardized incidence rate.
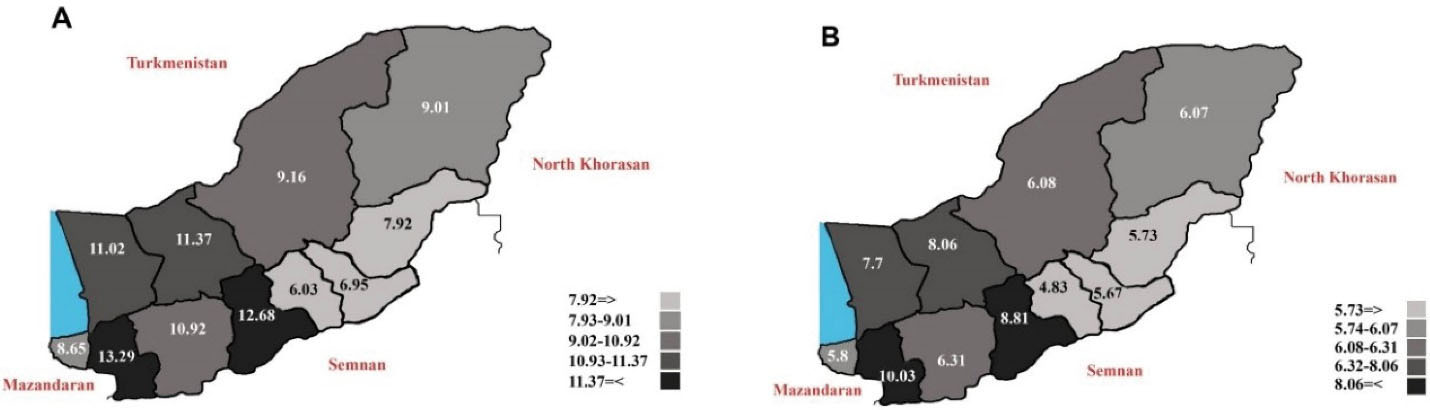
Figure 4.
Age Standardized Incidence Rate (Per 100 000 Person-Year) of Leukemia in Golestan Cities (2004–2017). A = Male, B = Female.
.
Age Standardized Incidence Rate (Per 100 000 Person-Year) of Leukemia in Golestan Cities (2004–2017). A = Male, B = Female.
Discussion
This study investigated the incidence and time trends of leukemia and MM in the Golestan province of Northern Iran during 2004–2017.
Our study demonstrated elevated ASRs for leukemia (11.50 and 6.70 per 100 000 in males and females, respectively) in comparison with the national average (8.32 and 5.40 in males and females, respectively).20 Based on the GLOBOCAN 2018, the Global incidence rates of leukemia in males and females were 6.10 and 4.30, respectively.12
Our findings also suggested that the incidence rates of MM in Golestan were 2.80 and 2.10 per 100 000 in males and females, respectively. Based on a report of the Iranian national cancer registry, the incidence rates of MM were 2.64 and 1.73 per 100 000 in Iranian males and females, respectively.20 Based on GLOBOCAN 2018, the global incidence rates of MM were 2.10 and 1.40 in male and females, respectively.12 Another study in Iran estimated the incidence rate of MM at 2.00 and 1.20 in males and females, respectively.21 The results of a study from China similarly showed that the incidence rate of MM was 1.84 per 100 000 person-years for males and 1.30 for females.22 Therefore, according to our results, it seems that the incidence rates of leukemia and MM in our population are higher than national and even the global averages, suggesting the need to study the risk factors and clarify the reasons for these high rates in our population.
Our results suggested higher incidence rates of leukemia and MM in males than females. This finding is in agreement with a previous report from other populations in Iran and other countries.23-25 Increased rates of leukemia and MM in males might be attributable to a higher prevalence of cigarette smoking,26 higher body mass index,27 occupational exposure,28 environmental carcinogens29 and, exposure to specific pesticides.30
In light of the results, we noticed an increasing trend in the incidence rate of leukemia in the urban population, which may be due to lifestyle modification and environmental risk factors in urban areas, such as air pollution (especially long-term exposure to traffic‐related air pollution) during recent years.31,32 Another study in an industrial area in northern Italy suggested a possible role for environmental air pollution from industrial sites regarding the risk of leukemia in adult populations.33 Ease of access to healthcare services and addressing the diagnostic gap of malignancies in urban areas may also be considered as possible explanation for their increasing trends in our urban population. Further studies are needed to clarify the reasons for the increasing trend in the incidence of leukemia in the urban population of Golestan, Iran.
Based on our findings, the incidence rate of leukemia was higher in central and western parts of the Golestan province. Other studies from Japan,34 Spain35 and Mexico36 similarly suggest geographical disparities in the incidence of leukemia. These differences may be attributed to differences in the prevalence of genetic or environmental factors, including ionizing radiation, non-ionizing radiation, pesticides, parental exposure, and infections.36 The higher rate of urbanization and its related risk factors in the western and central part of the province may also partly explain the higher incidence of leukemia in these parts of the Golestan province. Further investigations should be conducted to clarify the reasons for the higher incidence of leukemia in certain areas of the Golestan province.
In this study, we obtained data on leukemia and MM from the GPCR dataset, which is a high-quality population-based cancer registry and a voting member of the IACR. Benefitting from the high quality GPCR was the major strength of our study. As in other similar population-based cancer registries, data on risk factors were not available in the GPCR dataset. Therefore, we could not clarify the reasons for time trends and geographical disparities in the incidence of leukemia and MM in the Golestan population. This was a limitation of the present study and should be addressed in future projects.
In conclusion, we found that the incidence rates of leukemia and MM tend to be elevated in Golestan, Northern Iran, compared with national and global averages. Our results showed a male preponderance in leukemia rates as well as elevated rates in central and western parts of Golestan. We found increasing trends in the incidence of leukemia in the urban population. High prevalence of risk factors including cigarette smoking, higher body mass index in males and exposure to occupational and environmental carcinogens including pesticides may partly explain the high rates and increasing trends in the incidence of leukemia and MM in the Golestan province. Further investigations are warranted to clarify and validate the reasons for the geographical disparities and time trends of these malignancies in our population.
Supplementary Materials
Supplementary file 1 contains Table S1.
(pdf)
Acknowledgements
The authors greatly appreciate the great contribution and efforts of the GPCR staff and all physicians and healthcare personnel in the GPCR sources for their help and support in data collection and quality control. This project was funded by the Golestan University of Medical Sciences under contract 35-78724.
Authors’ Contribution
NJ-D collaborated in data processing; collaborated in analysis; wrote the manuscript. MN-T, MF and SMS collaborated in data collection; critically reviewed manuscript. SRK and FGK edited, critically reviewed manuscript and collaborated in quality control. RD contributed to interpretation of findings, edited and critically reviewed manuscript. AP conceptualized and designed the study; edited and critically reviewed manuscript. GR performed statistical analysis and wrote the manuscript. All authors read and approved the final manuscript.
Conflict of Interest Disclosures
The authors declare that they have no conflict of interest.
Ethical Statement
The protocol of this study was reviewed and approved by the Ethics Committee of Golestan University of medical sciences (ethics code: IR.GOUMS.REC.1396.298).
References
- Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol 2012; 13(8):790-801. doi: 10.1016/s1470-2045(12)70211-5 [Crossref] [ Google Scholar]
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011; 61(2):69-90. doi: 10.3322/caac.20107 [Crossref] [ Google Scholar]
- Castillo JJ, Mull N, Reagan JL, Nemr S, Mitri J. Increased incidence of non-Hodgkin lymphoma, leukemia, and myeloma in patients with diabetes mellitus type 2: a meta-analysis of observational studies. Blood 2012; 119(21):4845-50. doi: 10.1182/blood-2011-06-362830 [Crossref] [ Google Scholar]
- Koohi F, Salehiniya H, Shamlou R, Eslami S, Mahery Ghojogh Z, Kor Y. Leukemia in Iran: epidemiology and morphology trends. Asian Pac J Cancer Prev 2015; 16(17):7759-63. doi: 10.7314/apjcp.2015.16.17.7759 [Crossref] [ Google Scholar]
- Rodriguez-Abreu D, Bordoni A, Zucca E. Epidemiology of hematological malignancies. Ann Oncol 2007; 18 Suppl 1:i3-i8. doi: 10.1093/annonc/mdl443 [Crossref] [ Google Scholar]
- Wagner G, Fenchel K, Back W, Schulz A, Sachse MM. Leukemia cutis - epidemiology, clinical presentation, and differential diagnoses. J Dtsch Dermatol Ges 2012; 10(1):27-36. doi: 10.1111/j.1610-0387.2011.07842.x [Crossref] [ Google Scholar]
- Büchner T, Saußele S, Hehlmann R. Akute und chronische myeloische Leukämie. In: Dietel M, Suttorp N, Zeitz M, eds. Harrisons Innere Medizin. Vol 1. Berlin: ABW Wissenschaftsverlag; 2009.
- Pezzutto A, Dörken B. Neoplasien des lymphatischen systems. In: Dietel M, Suttorp N, Zeitz M, eds. Harrisons Innere Medizin. Vol 1. Berlin: ABW Wissenschaftsverlag; 2009. p. 857-73.
- Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 2009; 114(5):937-51. doi: 10.1182/blood-2009-03-209262 [Crossref] [ Google Scholar]
- Kazandjian D. Multiple myeloma epidemiology and survival: A unique malignancy. Semin Oncol 2016; 43(6):676-81. doi: 10.1053/j.seminoncol.2016.11.004 [Crossref] [ Google Scholar]
- Egan JB, Shi CX, Tembe W, Christoforides A, Kurdoglu A, Sinari S. Whole-genome sequencing of multiple myeloma from diagnosis to plasma cell leukemia reveals genomic initiating events, evolution, and clonal tides. Blood 2012; 120(5):1060-6. doi: 10.1182/blood-2012-01-405977 [Crossref] [ Google Scholar]
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68(6):394-424. doi: 10.3322/caac.21492 [Crossref] [ Google Scholar]
- Rajabli N, Naeimi-Tabeie M, Jahangirrad A, Sedaghat SM, Semnani S, Roshandel G. Epidemiology of leukemia and multiple myeloma in Golestan, Iran. Asian Pac J Cancer Prev 2013; 14(4):2333-6. doi: 10.7314/apjcp.2013.14.4.2333 [Crossref] [ Google Scholar]
- Roshandel G, Semnani S, Fazel A, Honarvar M, Taziki M, Sedaghat S. Building cancer registries in a lower resource setting: the 10-year experience of Golestan, Northern Iran. Cancer Epidemiol 2018; 52:128-33. doi: 10.1016/j.canep.2017.12.014 [Crossref] [ Google Scholar]
- Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. International Classification of Diseases for Oncology. Geneva: International Agency for Research on Cancer; 2000.
- Hasanpour-Heidari S, Fazel A, Semnani S, Khandoozi SR, Amiriani T, Sedaghat S. Temporal and geographical variations in colorectal cancer incidence in Northern Iran 2004-2013. Cancer Epidemiol 2019; 59:143-7. doi: 10.1016/j.canep.2019.02.003 [Crossref] [ Google Scholar]
- Jafari-Delouei N, Naeimi-Tabiei M, Fazel A, Ashaari M, Hatami E, Sedaghat SM. Descriptive epidemiology of lymphoma in Northern Iran: results from the Golestan registry 2004-2013. Arch Iran Med 2020; 23(3):150-4. [ Google Scholar]
- Segi M. Cancer Mortality for Selected Sites in 24 Countries (1950-57). Sendai, Japan: Department of Public Health, Tohoku University of Medicine; 1960.
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19(3):335-51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z [Crossref] [ Google Scholar]
- Roshandel G, Ghanbari-Motlagh A, Partovipour E, Salavati F, Hasanpour-Heidari S, Mohammadi G. Cancer incidence in Iran in 2014: results of the Iranian National Population-based Cancer Registry. Cancer Epidemiol 2019; 61:50-8. doi: 10.1016/j.canep.2019.05.009 [Crossref] [ Google Scholar]
- Almasi Z, Mohammadian-Hafshejani A, Salehiniya H. Incidence, mortality, and epidemiological aspects of cancers in Iran; differences with the world data. J BUON 2016; 21(4):994-1004. [ Google Scholar]
- Wang S, Xu L, Feng J, Liu Y, Liu L, Wang J. Prevalence and incidence of multiple myeloma in urban area in China: a national population-based analysis. Front Oncol 2019; 9:1513. doi: 10.3389/fonc.2019.01513 [Crossref] [ Google Scholar]
- Chen W, Zheng R, Zuo T, Zeng H, Zhang S, He J. National cancer incidence and mortality in China, 2012. Chin J Cancer Res 2016; 28(1):1-11. doi: 10.3978/j.issn.1000-9604.2016.02.08 [Crossref] [ Google Scholar]
- Novak I, Jaksić O, Kulis T, Batinjan K, Znaor A. Incidence and mortality trends of leukemia and lymphoma in Croatia, 1988-2009. Croat Med J 2012; 53(2):115-23. doi: 10.3325/cmj.2012.53.115 [Crossref] [ Google Scholar]
- Miranda-Filho A, Piñeros M, Ferlay J, Soerjomataram I, Monnereau A, Bray F. Epidemiological patterns of leukaemia in 184 countries: a population-based study. Lancet Haematol 2018; 5(1):e14-e24. doi: 10.1016/s2352-3026(17)30232-6 [Crossref] [ Google Scholar]
- Xu X, Talbott EO, Zborowski JV, Rager JR. Cigarette smoking and the risk of adult leukemia: results from the Three Mile Island cohort study. Arch Environ Occup Health 2007; 62(3):131-7. doi: 10.3200/aeoh.62.3.131-137 [Crossref] [ Google Scholar]
- Larsson SC, Wolk A. Overweight and obesity and incidence of leukemia: a meta-analysis of cohort studies. Int J Cancer 2008; 122(6):1418-21. doi: 10.1002/ijc.23176 [Crossref] [ Google Scholar]
- Adegoke OJ, Blair A, Shu XO, Sanderson M, Jin F, Dosemeci M. Occupational history and exposure and the risk of adult leukemia in Shanghai. Ann Epidemiol 2003; 13(7):485-94. doi: 10.1016/s1047-2797(03)00037-1 [Crossref] [ Google Scholar]
- Rathee R, Vashist M, Kumar A, Singh S. Incidence of acute and chronic forms of leukemia in Haryana. Int J Pharm Pharm Sci 2014; 6(2):323-5. [ Google Scholar]
- Alavanja MC, Bonner MR. Occupational pesticide exposures and cancer risk: a review. J Toxicol Environ Health B Crit Rev 2012; 15(4):238-63. doi: 10.1080/10937404.2012.632358 [Crossref] [ Google Scholar]
- Dehghani M, Keshtgar L, Javaheri MR, Derakhshan Z, Oliveri Conti G, Zuccarello P. The effects of air pollutants on the mortality rate of lung cancer and leukemia. Mol Med Rep 2017; 15(5):3390-7. doi: 10.3892/mmr.2017.6387 [Crossref] [ Google Scholar]
- Raaschou-Nielsen O, Ketzel M, Harbo Poulsen A, Sørensen M. Traffic-related air pollution and risk for leukaemia of an adult population. Int J Cancer 2016; 138(5):1111-7. doi: 10.1002/ijc.29867 [Crossref] [ Google Scholar]
- Parodi S, Santi I, Casella C, Puppo A, Montanaro F, Fontana V. Risk of leukaemia and residential exposure to air pollution in an industrial area in Northern Italy: a case-control study. Int J Environ Health Res 2015; 25(4):393-404. doi: 10.1080/09603123.2014.958136 [Crossref] [ Google Scholar]
- Tajima K, Tominaga S. Epidemiology of adult T-cell leukemia/lymphoma in Japan. Curr Top Microbiol Immunol 1985; 115:53-66. doi: 10.1007/978-3-642-70113-9_4 [Crossref] [ Google Scholar]
- Sierra M, Alonso A, Odero MD, Gonzalez MB, Lahortiga I, Pérez JJ. Geographic differences in the incidence of cytogenetic abnormalities of acute myelogenous leukemia (AML) in Spain. Leuk Res 2006; 30(8):943-8. doi: 10.1016/j.leukres.2005.12.025 [Crossref] [ Google Scholar]
- Tlacuilo-Parra A, Garibaldi-Covarrubias R, Romo-Rubio H, Soto-Sumuano L, Ruiz-Chávez CF, Suárez-Arredondo M. Geographical distribution and cluster detection of childhood leukemia in the metropolitan area of Guadalajara, Mexico. Rev Invest Clin 2017; 69(3):159-65. doi: 10.24875/ric.17002131 [Crossref] [ Google Scholar]