Arch Iran Med. 24(11):796-803.
doi: 10.34172/aim.2021.119
Original Article
Reperfusion Therapy and Predictors of 30-Day Mortality after ST-Segment Elevation Myocardial Infarction in a University Medical Center in Western Iran
Nahid Salehi 1  , Sayeh Motevaseli 1, Parisa Janjani 1, Mostafa Bahremand 1, Reza Heidari Moghadam 1, Mohammad Rouzbahani 1, Soraya Siabani 2, Hooman Tadbiri 3, Mahdi Nalini 1, *
, Sayeh Motevaseli 1, Parisa Janjani 1, Mostafa Bahremand 1, Reza Heidari Moghadam 1, Mohammad Rouzbahani 1, Soraya Siabani 2, Hooman Tadbiri 3, Mahdi Nalini 1, * 
Author information:
1Cardiovascular Research Center, Health Institute, Imam-Ali hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran
2Department of Health Education and Health Promotion, Kermanshah University of Medical Sciences, Kermanshah, Iran
3Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
*Corresponding Author: Mahdi Nalini, MD, PhD; Cardiovascular Research Center, Imam-Ali hospital, Shahid Beheshti Blvd., Kermanshah 6715847145, Iran. Phone: +98-9183366132. Email:
mahdinalini@yahoo.com
Abstract
Background:
Considerable variability in survival rate after ST-segment elevation myocardial infarction (STEMI) is present and outcomes remain suboptimal, especially in low- and middle-income contraries. This study aimed to investigate predictors of 30- day mortality after STEMI, including reperfusion therapy, in a tertiary hospital in western Iran.
Methods:
In this registry-based cohort study (2016–2019), we investigated reperfusion therapies – primary percutaneous coronary intervention (PPCI), pharmaco-invasive (thrombolysis followed by angiography/percutaneous coronary intervention), and thrombolysis alone – used in Imam-Ali hospital, the only hospital with a PPCI capability in the Kermanshah Province. We estimated hazard ratios (HRs) and 95% confidence intervals (CIs), using Cox proportional-hazard models, to investigate the potential predictors of 30-day mortality including reperfusion therapy, admission types (direct admission/referral from non-PPCI-capable hospitals), demographic variables, coronary risk factors, vital signs on admission, medical history, and laboratory tests.
Results:
Data of 2428 STEMI patients (mean age: 60.73; 22.9% female) were available. Reperfusion therapy was performed in 84% of patients (58% PPCI, 10% pharmaco-invasive, 16% thrombolysis alone). Only 17% of the referred patients had received thrombolysis at non-PPCI-capable hospitals. Among patients with thrombolysis, only 38.2% underwent coronary angiography/ percutaneous coronary intervention. The independent predictors of mortality were: no reperfusion therapy (HR: 2.01, 95% CI: 1.36–2.97), referral from non-PPCI-capable hospitals (1.73, 1.22–2.46), age (1.03, 1.01–1.04), glomerular filtration rate (0.97, 0.96–0.97), heart rate>100 bpm (1.94, 1.22–3.08), and systolic blood pressure<100 mm Hg (4.92, 3.43–7.04). Mortality was lower with the pharmaco-invasive approach, although statistically non-significant, than other reperfusion therapies.
Conclusion:
Reperfusion therapy, admission types, age, glomerular filtration rate, heart rate, and blood pressure were independently associated with 30-day mortality. Using a comprehensive STEMI network to increase reperfusion therapy, especially pharmaco-invasive therapy, is recommended.
Keywords: Death, Myocardial reperfusion, Percutaneous coronary intervention, Risk factors, ST elevation myocardial infarction
Copyright and License Information
© 2021 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Salehi N, Motevaseli S, Janjani P, Bahremand M, Heidari Moghadam R, Rouzbahani M, et al. Reperfusion therapy and predictors of 30-day mortality after st-segment elevation myocardial infarction in a university medical center in western iran. Arch Iran Med. 2021;24(11):796-803. doi: 10.34172/aim.2021.119
Introduction
Ischemic heart disease is the single most common cause of death worldwide, accounting for 16.17% of global deaths.1 In 2019, it was the main cause of 9.14 million deaths and 182 million disability-adjusted life years, with a global prevalence of 197 million cases.2 In Iran, ischemic heart disease is the leading cause of death, accounting for 26.28% of total deaths.1 Acute coronary syndrome including ST-segment elevation myocardial infarction (STEMI) may be the first manifestation of ischemic heart disease with substantial morbidity and mortality.3
Regional differences exist in treatment strategies and mortality rates attributed to STEMI within and across countries, suggesting opportunities for performance improvement.4 Widespread use of modern reperfusion therapies including primary percutaneous coronary intervention (PPCI), thrombolysis, and pharmaco-invasive (i.e. thrombolysis followed by angiography and, if indicated, percutaneous coronary intervention [PCI]), has resulted in a fall in STEMI mortality, particularly in developed countries5; however, in low- and middle-income countries (LMICs), where 80% of all cardiovascular deaths occur, lack of an appropriate care system is the most important barrier to implementing guideline-based STEMI treatment.6 A considerable number of STEMI patients, especially in LMICs, are not offered any reperfusion therapy, particularly PPCI which is the preferred reperfusion strategy in STEMI patients.5 A study in China showed that the in-hospital mortality rate of STEMI in county-level hospitals was 3-times higher than province-level hospitals (10.2% vs. 3.1%, respectively), partly due to hospital facilities and reperfusion therapy.7
There is no consensus on the predictors of short-term mortality of STEMI.8 STEMI mortality may be influenced by many health-system level and individual level factors such as time delay to treatment, ambulance system efficacy, reperfusion strategy, in-hospital treatment, age, previous heart disease, renal function, number of diseased coronary arteries, and known risk factors including diabetes mellitus, hypertension, dyslipidemia, and tobacco smoking.8,9
Little is known about the management and mortality predictors of STEMI in LMICs. Imam-Ali hospital is the only tertiary care academic cardiovascular center in the Kermanshah Province in western Iran. It is also the only hospital in the province with a 24 hours a day, 7 days a week (24/7) PPCI capability. The present study investigates the predictors of 30-day mortality of STEMI patients, including their received reperfusion therapies, in this hospital.
Materials and Methods
Study Setting, Design and Participants
The Kermanshah province in western Iran had 1 952 434 inhabitants in the 2016 census in its area of 25 009 km2.10 There are 23 hospitals in all 14 counties of this province; 13 of them are in the city of Kermanshah, the province capital.10 The geographical distribution of hospitals in the province is shown in Figure 1. Imam-Ali hospital is a cardiology training center in the city of Kermanshah, affiliated to the Kermanshah University of Medical Sciences. This is the only 24/7 PPCI-capable hospital in the province. Other hospitals in the province are non-PPCI capable but have been equipped to provide thrombolytic therapy. Ambulance services in this province are not equipped with electrocardiography machines and thrombolysis facilities.
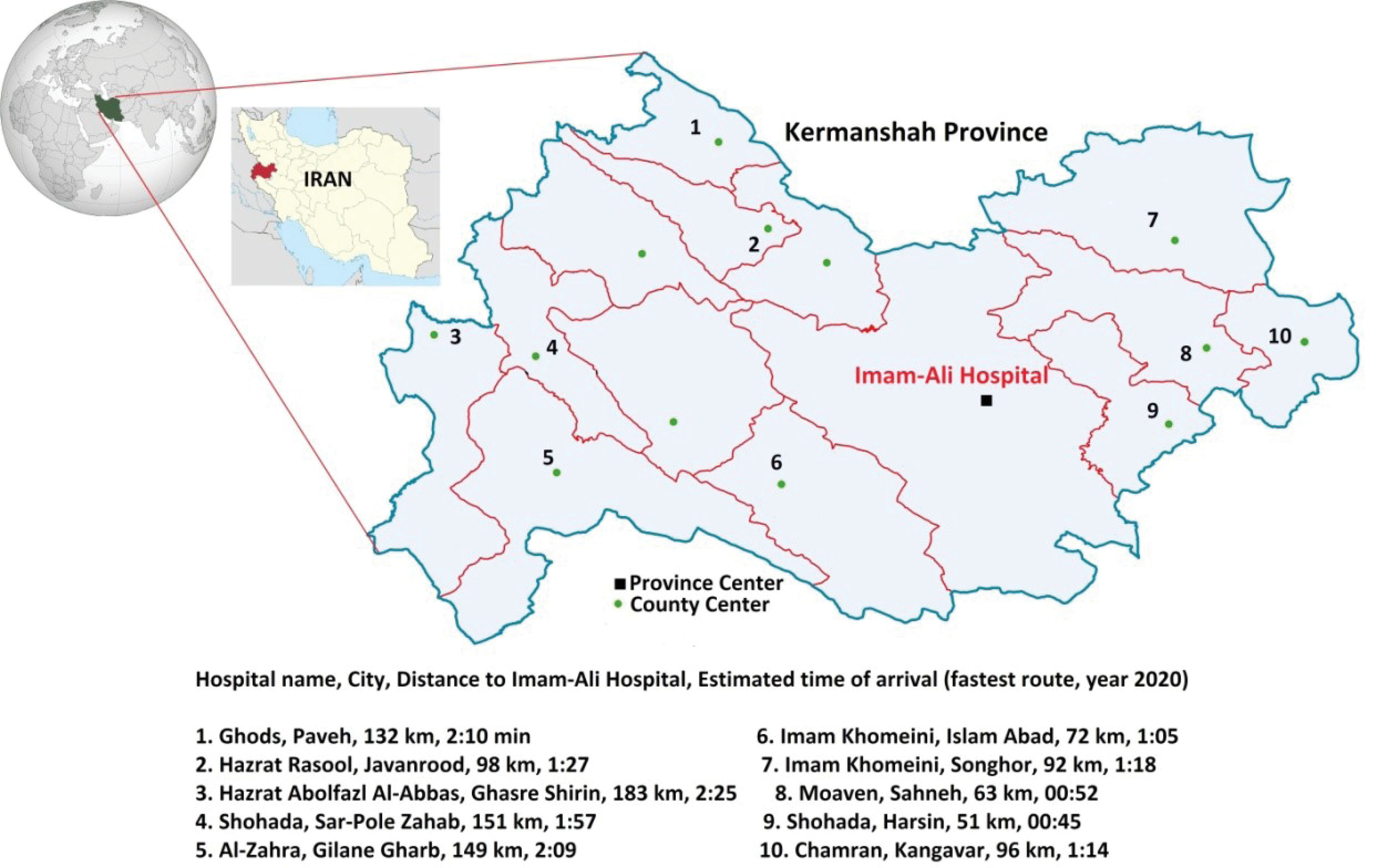
Figure 1.
Estimated Driving Distances from County Hospitals to Imam-Ali Hospital, the Only Primary Percutaneous Coronary Intervention Capable Hospital in Kermanshah Province. Driving distances are estimated using Goggle Maps (https://www.google.com/maps).
.
Estimated Driving Distances from County Hospitals to Imam-Ali Hospital, the Only Primary Percutaneous Coronary Intervention Capable Hospital in Kermanshah Province. Driving distances are estimated using Goggle Maps (https://www.google.com/maps).
This registry-based cohort study included all adult patients (> 18 years) who presented with STEMI to Imam-Ali hospital from July 1, 2016 to September 19, 2019. Diagnosis was made by cardiologists based on current guidelines.11 The STEMI patients who were hospitalized more than 24-hours before referring to Imam-Ali hospital were excluded from this registry. In this study, we also excluded patients with out-of-hospital cardiac arrest. The eligible patients were followed up 30 days after STEMI events. All participants signed written informed consent.
Baseline Assessment
In the registry, trained physicians and nurses collected demographic and clinical data such as past medical history, the time of the onset of symptoms, and transfer to Imam-Ali hospital, from personal interviews with patients and/or their attendants. Direct admission (self-presentation) to Imam-Ali hospital or referral from other hospitals was recorded. The time between symptom onset and arrival to hospital (onset-to-arrival time) were calculated. History of cardiovascular events (previous myocardial infarction, stroke, or chronic heart failure), coronary intervention (PCI or coronary artery bypass graft surgery), diabetes, and hypertension were recorded, based on self-reports of confirmed diagnoses by health care members. We recorded the reperfusion treatment used including: PPCI, pharmaco-invasive, thrombolysis alone, and none (no reperfusion). Thrombolysis was received either before or after admission at Imam-Ali hospital. Information about the admission process, hemodynamic status, electrocardiography data, medical treatment, laboratory tests, etc. was obtained from hospital medical records. Systolic blood pressure (SBP) and heart rate (HR) were measured on admission at Imam-Ali hospital and categorized into two groups (SBP: < 100/ ≥ 100 mm Hg and HR: > 100/ ≤ 100 bmp, respectively), based on the categories of thrombolysis in myocardial infarction (TIMI) risk score.12 Body-mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Lipid profile and creatinine level were measured on the first day of admission. We defined high low-density lipoprotein cholesterol (LDL-C) as LDL-C > 160 mg/dL and low high-density lipoprotein cholesterol (HDL-C) as HDL-C < 40 mg/dL in men and HDL-C < 50 mg/dL in women.13 We estimated glomerular filtration rate (GFR) using the CKD-EPT equation,14 based on patients’ initial serum creatinine level. All recorded data were quality controlled by trained physicians.
Study Outcome and Follow-up
The main outcome was 30-day mortality after STEMI. Data of in-hospital mortality were collected using hospital records. Upon hospital admission, patients’ mobile phone numbers and home phone numbers, as well as two phone numbers of their family members or their attendants were recorded. Trained nurses contacted each patient by phone and collected information about their vital status. If death occurred within 30 days after STEMI, the cause and date of death were recorded. Follow-up time extended from the date of STEMI diagnosis to the date of death, loss-to-follow up, or 30 days after STEMI, whichever came first.
Statistical Analysis
All statistical analyses were performed using Stata statistical software (Stata Corp, Release 12, College Station, TX). We used the registry data and included all eligible patients in the study, so we did not determine the sample size. Continuous variables were expressed as mean (SD) and discrete variables were presented as counts (percentages). Cox proportional-hazard modeling was performed to determine predictors of 30-day mortality. The proportionality of hazards was verified using Schoenfeld’s global test and log–log plots. Candidate variables for inclusion in the models were selected according to previously reported mortality predictors9,12 and variables of interest; including age (continues), sex (female/male), admission type (direct admission/referral), onset-to-arrival time (< 4, 4‒8, and > 8 hours), SBP (< 100/ ≥ 100 mm Hg), HR (> 100/ ≤ 100 bmp), history of cardiovascular events (yes/no), history of coronary intervention (yes/no), ever smoking (yes/no), diabetes (yes/no), hypertension (yes/no), type of MI (anterior wall or left bundle branch block/others), early reperfusion therapy (PPCI/pharmaco-invasive/thrombolysis/no-reperfusion), GFR (continuous), BMI (continuous), high LDL-C (yes/no), and low HDL-C (yes/no). We reported HRs with 95% confidence intervals (95% CIs) using univariable, age- and sex-adjusted, and fully-adjusted Cox proportional-hazards models. We used change-in-estimate strategies, with 10% change rule,15 to identify the independent predictors of 30-day mortality in the final model. We also used stepwise selection to confirm the final model. We performed a subgroup analysis based on the admission types – direct admission to Imam-Ali hospital and referral from other hospitals. In a sensitivity analysis, we included out-of-hospital cardiac arrests and re-evaluated the results. We performed all analyses on complete case data. P < 0.05 and 95% CIs not including one were considered as statistically significant.
Results
A total of 2469 patients with STEMI were admitted to Imam-Ali hospital between July 1, 2016 and September 19, 2019 (38.63 months). We excluded 41 patients with out-of-hospital cardiac arrests from the analysis, resulting in a final study population of 2428 patients. Rates of missing data among covariates were low, including onset-to-arrival time: 44 (1.81%), BMI: 40 (1.65%), SBP and HR on admission: 1(0.04%), serum creatinine: 3 (0.12%), LDL-C: 110 (4.53%), and HDL-C: 159 (6.55%). Nineteen patients (0.78%) were lost to follow-up to evaluate vital status after discharge.
Of 2428 patients, 1781 (73.35%) were directly admitted to Imam-Ali hospital and 647 (26.65%) were referred from other hospitals. Overall, 1412 (58.15%) patients received PPCI and 631(25.99%) received thrombolytic therapy. The use of PPCI was 219 per 1 000 000 inhabitants per year. Of 647 referred patients, 110 (17.00%) had received thrombolysis in non-PPCI-capable hospitals. Among 631 patients with thrombolytic therapy, 241 (38.2%) underwent pharmaco-invasive therapy (coronary angiography with or without PCI during hospitalization at Imam-Ali hospital).
The mean age of patients was 60.73 (SD: 12.44) years, and 22.86% were female. During 69,638 person-days of follow-up, 139 deaths were recorded, of which 123 (88.49%) occurred in hospital and 16 (11.51%) after discharge. The crude 30-day mortality rate was 5.72%. The baseline characteristics of the patients sorted by vital status are shown in Table 1.
Table 1.
Baseline Characteristics of STEMI Patients in Imam-Ali Hospital, Sorted by Vital Status
|
|
|
Patient Died
(n=139)
|
Patient Alive
(n=2289)
|
All
(n=2428)
|
|
Continuous Variables
|
| Age (years) |
|
69.27 (11.11) |
60.21 (12.33) |
60.73 (12.44) |
| Body mass index (kg/m2) |
|
25.17 (4.43) |
26.22 (4.02) |
26.18 (4.05) |
| Heart rate (bpm) |
|
78.95 (27.29) |
77.79 (19.76) |
77.85 (20.26) |
| Systolic blood pressure (mm Hg) |
|
115.31 (33.89) |
135.3 (29.15) |
134.16 (29.80) |
| GFR (mL/min per 1.73m2) |
|
51.03 (18.18) |
69.25 (17.54) |
68.22 (18.07) |
|
Categorical Variables
|
| Gender |
Female |
58 (41.73) |
497 (21.71) |
555 (22.86) |
| Male |
81 (58.27) |
1792 (78.29) |
1873 (77.14) |
| Ever Smoker |
Yes |
42 (30.22) |
1126 (49.19) |
1168 (48.11) |
| No |
97 (69.78) |
1163 (50.81) |
1260 (51.89) |
| Diabetes mellitus |
Yes |
41 (29.50) |
449 (19.62) |
490 (20.18) |
| No |
98 (70.50) |
1840 (80.38) |
1938 (79.82) |
| Hypertension |
Yes |
84 (60.43) |
931 (40.67) |
1015 (41.80) |
| No |
55 (39.57) |
1358 (59.33) |
1413 (58.20) |
| History of coronaryintervention |
Yes |
12 (8.63) |
207 (9.04) |
219 (9.02) |
| No |
127 (91.37) |
2082 (90.96) |
2209 (90.98) |
| History of cardiovascular events |
Yes |
37 (26.62) |
405 (17.69) |
442 (18.20) |
| No |
102 (73.38) |
1884 (82.31) |
1986 (81.80) |
| Direct admission to Imam-Ali hospital |
Yes |
80 (57.55) |
1701 (74.31) |
1781 (73.35) |
| No |
59 (42.45) |
588 (25.69) |
647 (26.65) |
| Time between symptom onset and admission (h) |
< 4 hours |
49 (51.58) |
1529 (66.80) |
1578 (66.19) |
| 4-8 hours |
22 (23.16) |
445 (19.44) |
467 (19.59) |
| > 8 hours |
24 (25.26) |
315 (13.76) |
339 (14.22) |
| HR > 100 bpm |
Yes |
23 (16.55) |
173 (7.56) |
196 (8.08) |
| No |
116 (83.45) |
2115 (92.44) |
2231 (91.92) |
| SBP < 100 mm Hg |
Yes |
49 (35.25) |
171 (7.47) |
220 (9.06) |
| No |
90 (64.75) |
2117 (92.53) |
2207 (90.94) |
| Anterior MI/LBBB |
Yes |
71 (51.08) |
1192 (52.08) |
1263 (52.02) |
| No |
68 (48.92) |
1097 (47.92) |
1165 (47.98) |
| High LDL-C* |
Yes |
6 (5.50) |
129 (5.84) |
135 (5.82) |
| No |
103 (94.50) |
2080 (94.16) |
2183 (94.18) |
| Low HDL-C** |
Yes |
71 (68.93) |
1187 (54.80) |
1258 (55.44) |
| No |
32 (31.07) |
979 (45.20) |
1011 (44.56) |
| Reperfusion therapy |
PPCI |
61 (43.88) |
1351 (59.02) |
1412 (58.15) |
| Pharmaco-invasive |
4 (2.88) |
237 (10.35) |
241 (9.93) |
| Thrombolysis alone |
23 (16.55) |
367 (16.03) |
390 (16.06) |
| No reperfusion |
51 (36.69) |
334 (14.59) |
385 (15.86) |
Data are mean (SD) or number (%). Percentages were calculated on the basis of participants with available data.
STEMI, ST-segment elevation myocardial infarction; MI, Myocardial infarction; LBBB, Left bundle branch block; HDL-C, High-density lipoprotein cholesterol; LDL-C, Low-density lipoprotein cholesterol; GFR, Glomerular filtration rate; PPCI, Primary percutaneous coronary intervention; HR, heart rate; SBP, Systolic blood pressure.
*LDL-C > 160 mg/dL. **HDL-C < 40 mg/dL in men and HDL-C < 50 mg/dL in women.
In crude analyses, older age, female sex, diabetes, hypertension, history of cardiovascular events, referral from other hospitals, SBP < 100 mm Hg, HR > 100 bpm, low GFR, low HDL-C, high onset-to-arrival time, and no reperfusion therapy increased the risk of death significantly. High BMI and ever smoking were protective factors of mortality in crude analyses; however, after adjusting for age and sex, their significant associations disappeared. Pharmaco-invasive therapy tended to be more protective than PPCI, although this association was not statistically significant (Table 2).
Table 2.
Risk Factors Associated with 30-Day Mortality of STEMI Patients in Imam-Ali Hospital
|
|
Crude HRs (95% CIs)
|
P
Value
|
Age- and Sex-Adjusted
HRs (95% CIs)
|
P
Value
|
Fully-Adjusted
HRs (95% CIs)
|
P
Value
|
| Age (y) |
1.06 (1.04–1.07) |
< 0.001 |
1.05 (1.04–1.07) |
< 0.001 |
1.02 (1.00–1.04) |
0.081 |
| Female sex |
2.47 (1.76–3.46) |
< 0.001 |
1.81 (1.29–2.56) |
0.001 |
1.36 (0.81–2.27) |
0.241 |
| Ever smoker |
0.46 (0.32–0.66) |
< 0.001 |
0.73 (0.49–1.09) |
0.121 |
1.07 (0.65–1.78) |
0.791 |
| Diabetes mellitus |
1.68 (1.17–2.42) |
0.005 |
1.46 (1.00–2.12) |
0.050 |
0.98 (0.58–1.66) |
0.943 |
| Hypertension |
2.16 (1.54–3.03) |
< 0.001 |
1.35 (0.94–1.93) |
0.104 |
1.44(0.88–2.36) |
0.141 |
| History of coronary intervention |
0.95 (0.53–1.72) |
0.867 |
1.03 (0.57–1.86) |
0.929 |
0.98 (0.42–2.30) |
0.961 |
| History of cardiovascular events |
1.65 (1.14–2.41) |
0.009 |
1.41 (0.97–2.06) |
0.072 |
0.92 (0.53–1.61) |
0.773 |
| Body mass index |
0.94 (0.89–0.99) |
0.011 |
0.97 (0.92–1.02) |
0.221 |
0.97 (0.91–1.03) |
0.316 |
| Referral from non-PPCI-capable hospitals |
2.06 (1.47–2.88) |
< 0.001 |
2.15 (1.54–3.02) |
< 0.001 |
2.47 (1.52–3.99) |
< 0.001 |
| Heart rate > 100 bpm |
2.32 (1.48–3.63) |
< 0.001 |
2.27 (1.45–3.56) |
< 0.001 |
1.78 (0.98–3.24) |
0.059 |
| Systolic blood pressure < 100 mm Hg |
5.98 (4.22–8.46) |
< 0.001 |
5.78 (4.08–8.20) |
< 0.001 |
4.01 (2.41–6.67) |
< 0.001 |
| Anterior MI/LBBB |
0.96 (0.69–1.34) |
0.810 |
0.96 (0.69–1.35) |
0.831 |
1.20 (0.76–1.89) |
0.436 |
| GFR (mL/min per 1.73m2) |
0.95 (0.94–0.96) |
< 0.001 |
0.96 (0.95–0.97) |
< 0.001 |
0.96 (0.95–0.98) |
< 0.001 |
| High LDL-C* |
0.94 (0.41–2.15) |
0.890 |
1.02 (0.45–2.33) |
0.962 |
1.02 (0.40–2.59) |
0.963 |
| Low HDL-C** |
1.80(1.19–2.73) |
0.006 |
1.49 (0.97–2.29) |
0.071 |
1.16 (0.71–1.85) |
0.551 |
| Time between symptom onset and admission (Reference: < 4 hours) |
|
|
|
|
|
|
| 4–8 hours |
1.53 (0.92–2.53) |
0.099 |
1.31 (0.79–2.18) |
0.290 |
0.93 (0.53–1.65) |
0.808 |
| > 8 hours |
2.33 (1.43–3.79) |
0.001 |
2.02 (1.24–3.30) |
0.005 |
0.91 (0.50–1.65) |
0.747 |
| Reperfusion therapy (Reference: PPCI) |
|
|
|
|
|
|
| Pharmaco-invasive |
0.38 (0.14–1.04) |
0.060 |
0.42 (0.15–1.17) |
0.097 |
0.61 (0.21–1.73) |
0.351 |
| Thrombolysis |
1.37 (0.85–2.21) |
0.199 |
1.34 (0.83–2.17) |
0.226 |
1.29 (0.71–2.33) |
0.406 |
| No reperfusion |
3.18 (2.19–4.61) |
< 0.001 |
2.40 (1.64–3.52) |
< 0.001 |
2.00 (1.20–3.36) |
0.008 |
STEMI, ST-segment elevation myocardial infarction; HR, Hazard ratio; CI, Confidence interval; MI, Myocardial infarction; LBBB, Left bundle branch block; HDL-C, High-density lipoprotein cholesterol; LDL-C, Low-density lipoprotein cholesterol; GFR, Glomerular filtration rate; PPCI, Primary percutaneous coronary intervention.
*LDL-C > 160mg/dL. **HDL-C < 40mg/dL in men and HDL-C < 50mg/dL in women.
Table 3 shows the independent predictors of 30-day mortality based on the multivariable analysis. In this model, the association of age, HR, SBP, referral from other hospitals, no reperfusion therapy, and GFR remained statistically significant. Overall, patients who received reperfusion therapy had a 59% lower rate of 30-day mortality (HR: 0.41, 95% CI: 0.29‒0.56). Subgroup analysis showed the same results in patients with direct admission and those who referred from other hospitals (Table 4). In the sensitivity analysis, out-of-hospital cardiac arrests had the strongest association with 30-day mortality with an HR (95% CI) of 4.92 (2.95‒8.21) in the final model. Age, referral from other hospitals, SBP < 100 mm Hg on admission, low GFR, type of MI (anterior wall or left bundle branch block), and no reperfusion therapy were also associated with increased mortality (see Table S1 of Supplementary file 1).
Table 3.
Final Multivariable Analysis of Independent Factors Associated with 30-Day Mortality of STEMI Patients in Imam-Ali Hospital
|
|
HRs (95% CIs)
|
P
Value
|
| Age (y) |
1.03 (1.01–1.04) |
0.001 |
| Referral from non-PPCI-capable hospitals |
1.73 (1.22–2.46) |
0.002 |
| Heart rate > 100 bpm |
1.94 (1.22–3.08) |
0.005 |
| Systolic blood pressure < 100 mm Hg |
4.92 (3.43–7.04) |
< 0.001 |
| GFR (mL/min per 1.73 m2) |
0.97 (0.96–0.97) |
< 0.001 |
| Reperfusion therapy (reference: PPCI) |
|
|
| Pharmaco-invasive |
0.42 (0.15–1.17) |
0.097 |
| Thrombolysis |
1.20 (0.74–1.94) |
0.465 |
| No reperfusion |
2.01 (1.36–2.97) |
< 0.001 |
STEMI, ST-segment elevation myocardial infarction; HR, Hazard ratio; CI, Confidence interval; GFR, Glomerular filtration rate; PPCI, Primary percutaneous coronary intervention.
Table 4.
Factors Associated with 30-Day Mortality of STEMI Patients in Imam-Ali Hospital Based on the Type of Admission
|
|
Direct Admission to
Imam-Ali Hospital
|
Referral from Non-PPCI-
capable Hospitals
|
|
|
HRs (95% CIs)
|
P
Value
|
HRs (95% CIs)
|
P
Value
|
| Age (y) |
1.02 (1.00–1.05) |
0.037 |
1.03 (1.00–1.05) |
0.016 |
| Heart rate > 100 bpm |
2.47 (1.37–4.46) |
0.003 |
1.31 (0.62–2.80) |
0.478 |
| Systolic blood pressure < 100 mm Hg |
4.10 (2.47–6.81) |
< 0.001 |
6.41 (3.74–10.98) |
< 0.001 |
| GFR (ml/min per 1.73m2) |
0.96 (0.95–0.97) |
< 0.001 |
0.97 (0.95–0.98) |
< 0.001 |
| Reperfusion therapy (reference: PPCI) |
|
|
|
|
| Pharmaco-invasive |
0.20 (0.03–1.50) |
0.118 |
0.63 (0.19–2.11) |
0.455 |
| Thrombolysis |
0.99 (0.50–1.97) |
0.984 |
1.45 (0.72–2.91) |
0.299 |
| No reperfusion |
1.79 (1.05–3.03) |
0.031 |
2.37 (1.27–4.44) |
0.007 |
STEMI, ST-segment elevation myocardial infarction; HR, hazard ratio; CI, Confidence interval; GFR, Glomerular filtration rate; PPCI, Primary percutaneous coronary intervention.
In Figure 2, we compared all the subgroups of patients, based on both reperfusion therapies and admission types, and considered PPCI in directly admitted patients as the reference group. Referred patients compared with those who admitted directly to Imam-Ali hospital tended to have poorer prognoses, in all the related categories of reperfusion treatments. Figure 2 also demonstrates lower mortality rates, although statistically non-significant, of the pharmaco-invasive therapy compared with PPCI, for both admission types.
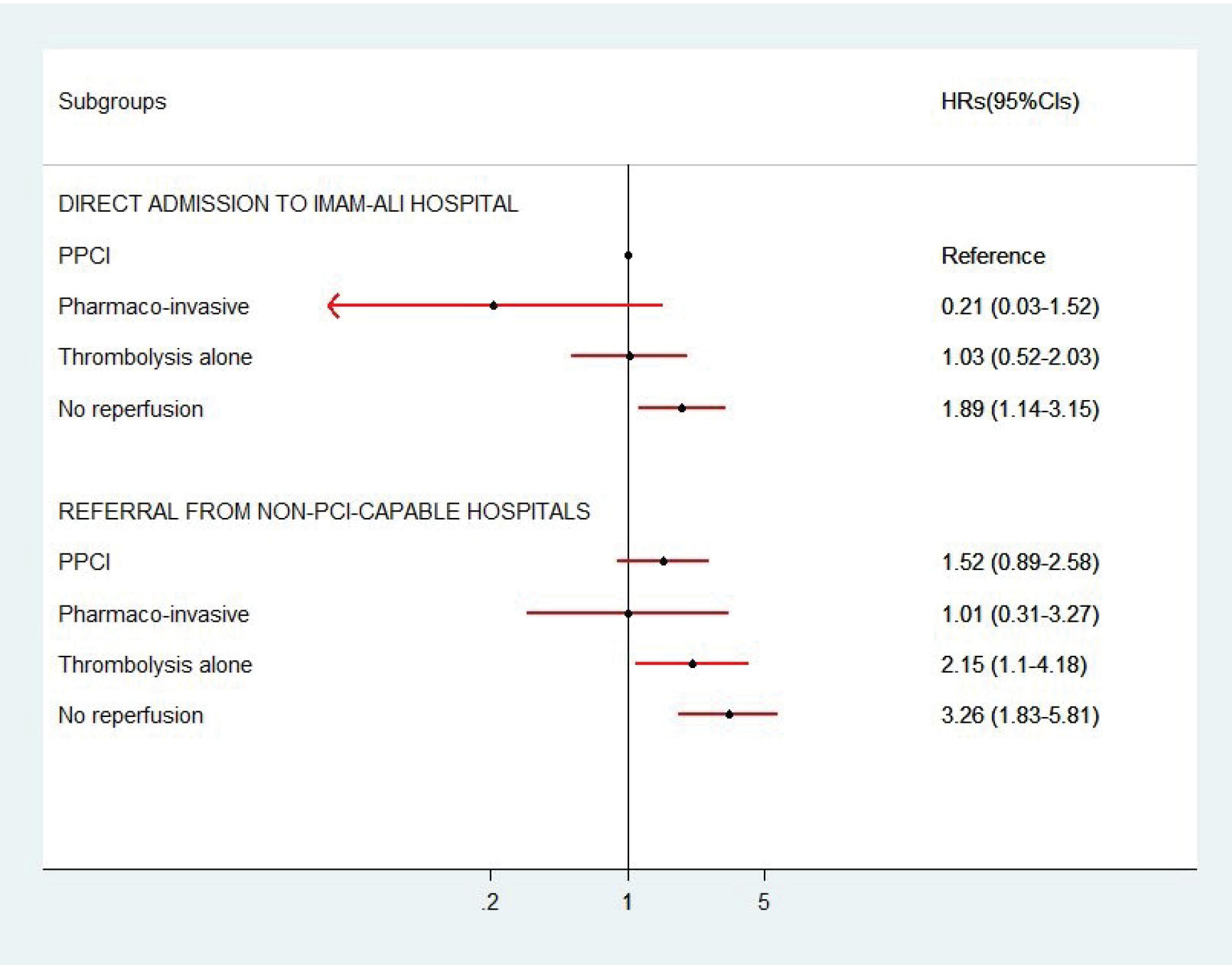
Figure 2.
Associations of Reperfusion Therapies with 30-Day Mortality in Patients with ST-Segment Myocardial Infarction Based on the Types of Admission (Direct Admission to Imam-Ali Hospital or Referral from Other Hospitals). Primary percutaneous coronary intervention (PPCI) in patients who directly admitted to Imam-Ali hospital is the reference group. Adjusted hazard ratios with 95% confidence intervals (HRs, 95% CIs), based on the final model, are presented.
.
Associations of Reperfusion Therapies with 30-Day Mortality in Patients with ST-Segment Myocardial Infarction Based on the Types of Admission (Direct Admission to Imam-Ali Hospital or Referral from Other Hospitals). Primary percutaneous coronary intervention (PPCI) in patients who directly admitted to Imam-Ali hospital is the reference group. Adjusted hazard ratios with 95% confidence intervals (HRs, 95% CIs), based on the final model, are presented.
Discussion
In the present study, 58% of patients received PPCI, 10% pharmaco-invasive, 16% thrombolysis alone, and 16% no reperfusion. Only 17% of patients referred to Imam-Ali hospital had received thrombolysis at non-PPCI-capable hospitals. Among patients with thrombolytic therapy, coronary angiography/PCI was reported in 38% of patients. The independent predictors of 30-day mortality after STEMI were lack of reperfusion therapy, referral from non-PPCI-capable hospitals, older age, lower GFR, and HR > 100 bpm or SBP < 100 mm Hg on admission.
In our study, early reperfusion therapy was associated with a 59% lower rate of 30-day mortality. Other studies have also reported that implementation of reperfusion therapy, particularly prompt PPCI (< 120 minutes) which is the preferred reperfusion strategy in STEMI patients, is associated with a reduced mortality rate.9 Although the guideline-based treatment in high-income countries has improved survival of STEMI patients, in LMICs, considerable healthcare resource and infrastructure constraints make implementing those guidelines unfeasible and thus, STEMI survival remains suboptimal.6 We showed that there are approximately 219 PPCI per 1 000 000 inhabitants annually, in the only 24/7 capable hospital in the province with almost two million population, much lower than 600 PPCI per 1 000 000 inhabitants in developed European countries such as Austria, Germany, and the Netherlands.5 The pharmaco-invasive strategy has been suggested as one of the most promising reperfusion strategies in LMICs.6 In our study, among 631 patients with thrombolytic therapy, only 38.2% received subsequent angiography with or without PCI. In some developed countries, using well-designed STEMI networks, almost all patients treated with thrombolytic therapy are directly transferred to PPCI-capable hospitals and undergo pharmaco-invasive therapy.16 In the current analysis, the mortality rate for the pharmaco-invasive approach was lower, although statistically non-significant, than other reperfusion therapy approaches. These results were seen in both subgroups of direct admission and referral to Imam-Ali hospital. Comparable survival rates between pharmaco-invasive and PPCI approaches have been reported in some other studies.17,18
We revealed that referral from non-PPCI capable hospitals was associated with a 73% increase in 30-day mortality rate compared with direct admission to Imam-Ali hospital, independent of the reperfusion therapies. This may be due to the lack of advanced hospital facilities and insufficient capabilities in clinical expertise in non-PPCI-capable hospitals in the province. A large study of STEMI patients in 108 hospitals in China investigated the variations in care and mortality among various levels of hospitals. The rates of reperfusion therapy and in-hospital mortality were 69.4% and 3.1% for province-level hospitals and 45.8% and 10.2% for county-level hospitals, respectively. More efforts to address the gaps in care and outcomes of STEMI for national quality improvement were recommended.7
Our primary results also demonstrated that older age, female sex, history of cardiovascular events, hypertension, diabetes, SBP < 100 mm Hg and/or HR > 100 bpm on admission, lower GFR, low HDL-C, and high onset-to-arrival time were associated with increased 30-day STEMI mortality, but in multivariable analyses, the associations remained statistically significant for age, HR, SBP, and GFR. Likewise, the TIMI risk score for STEMI was created based on the adjusted logistic regression models to predict 30-day mortality.12 Old age, female sex, diabetes, hypertension, HR > 100 bpm, SBP < 100 mm Hg, and previous cardiovascular diseases were among the final predictors of mortality.12 However, in the ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry–GWTG (Get With the Guidelines) study,19 significant associations with mortality were not reported for sex, diabetes, hypertension, and previous coronary intervention, in multivariable models. Similar to the Action Registry-GWTG study, we found that renal function was an independent predictor of mortality. For every one mL/min/1.73 m2 increase in GFR, the 30-day mortality rate decreased by 3% in our study. Renal function was not analyzed in the TIMI risk score study.12
In our study, 30-day mortality in never smokers was significantly higher than ever smokers; however, this association disappeared in the adjusted models. Smoking is one of the strongest risk factors for STEMI; however, some studies have shown that smokers have a favorable prognosis after acute myocardial infarction, known as “smoker’s paradox”.20,21 For example, in a study among 985,174 patients with STEMI undergoing PPCI, smokers had lower in-hospital mortality than non-smokers (2.0% vs. 5.9%).22 Another study showed a significant lower crude rate of death in smokers; however, after adjustment for age and other risk factors, smokers and non-smokers had similar mortality rates. Researchers revealed that smokers were 10 years younger than non-smokers with fewer cardiovascular risk factors.20 In fact, smoking is the strongest behavioral risk factor for the premature onset of atherosclerosis.23
Obesity is a known cardiovascular risk factor and nearly 70% of death related to high BMI are due to cardiovascular disease.24 However, there are conflicting data on the association between BMI and mortality in established coronary artery disease patients. Some,25,26 but not all,27 studies reported the protective effects of obesity; a phenomenon often termed the “obesity paradox”. We showed that higher BMI were associated with a decrease in 30-day mortality in our crude analysis, although these significant associations did not persist in age- and sex-adjusted and the final multivariable model. In a large population-based cohort study in Iran, BMI had a weak association with cardiovascular mortality.28 Researchers suggested using indicators of visceral adiposity, especially hip-adjusted waist circumference, as the best obesity indicator in that population. They argued that BMI cannot distinguish lean mass from fat mass and cannot recognize fat distribution in the body.28
To our knowledge, this is the first large registry-based study with detailed data about the 30-day mortality of STEMI patients during more than 3 years in western Iran. This study collected data from all consecutive eligible patients to minimize selection bias. The availability of data to adjust for confounders and the extremely low loss to follow-up rate were among other strengths of this study. However, the results of this study should be interpreted in the context of the following limitations. Firstly, the study was conducted in the only 24/7 PPCI-capable hospital in the Kermanshah province after excluding out-of-hospital cardiac arrests. Therefore, the results of mortality rates may not be applicable to the entire province or country. Although we showed a 5.7% crude mortality rate in PPCI-capable Imam-Ali hospital, a nationwide study reported an in-hospital mortality rate of 12.1%, in 31 provinces of Iran.29 In line with our results, in-hospital STEMI mortality rate in Tehran Heart Center (another PPCI-capable hospital in Iran) was 5.4% and reduced from 8% to 3.9% during 2006‒2017, mainly due to the improvement of reperfusion therapies.30 Secondly, we did not have data on all of the factors associated with 30-day mortality, as well as unmeasured confounding variables that may be present in any observational studies. Thirdly, as an observational study, we acknowledge information bias such as exposure identification bias and misclassification, especially about self-reported variables. Lastly, the small number of deaths in some reperfusion subgroups precluded further detailed analyses.
Conclusions and Implication
According to the findings of our study, no reperfusion therapy, referral from non-PPCI-capable hospitals, older age, lower GFR, and HR > 100 bpm or SBP < 100 mm Hg on admission were independently associated with increased 30-day mortality after STEMI. Our findings indicated the importance of immediate/management factors for the 30-day mortality of STEMI compared with the traditional long-term cardiovascular risk factors.
This study has important implications. Using an efficacious STEMI care network, efforts must be focused on widespread aspects of STEMI care in the entire province, such as improving hospital facilities, transportation systems, and intensive training in all parts of the health system, including PPCI-capable and non-PPCI-capable hospitals. Geographic limitations and resource constraints in the Kermanshah Province, as well as many other regions of LMICs, indicate that PPCI cannot be provided for most of the population; however, the pharmaco-invasive strategy can be considered as the best alternative and the most feasible pathway for STEMI treatment in such regions.6
Supplementary Materials
Supplementary file 1 contains Table S1.
(pdf)
Acknowledgements
The authors thank the Kermanshah University of Medical Sciences for funding this project. We wish to thank all the Imam-Ali hospital staff, especially the Cardiovascular Research Center, Dr. Hossein Siabani, Ms. Leila Zamzam, Mrs. Hanyeh Charejo and Ms. Elaheh Mohammadi for data gathering; without their contribution, this work would not have been accomplished.
Authors’ Contribution
Design and conception: SM and MN; data acquisition: SS, NS, RHM, PJ, MR, MB; analysis and interpretation: MN, HT, SM; and writing the manuscript MN, SM, HT. All authors critically revised the manuscript and gave final approval and agree to be accountable for all aspects of the paper.
Conflict of Interest Disclosures
The authors declare no conflict of interest.
Ethical Statement
The ethics committee of the Kermanshah University of Medical Sciences approved the study protocol (Ethics registration code: KUMS.REC.1395.252).
References
- Global Burden of Diseases. [Updated 2019; cited 1 Jan 2021]. Available from: https://vizhub.healthdata.org/gbd-compare/.
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol 2020; 76(25):2982-3021. doi: 10.1016/j.jacc.2020.11.010 [Crossref] [ Google Scholar]
- Anderson JL, Morrow DA. Acute myocardial infarction. N Engl J Med 2017; 376(21):2053-64. doi: 10.1056/NEJMra1606915 [Crossref] [ Google Scholar]
- Bradley EH, Curry LA, Spatz ES, Herrin J, Cherlin EJ, Curtis JP. Hospital strategies for reducing risk-standardized mortality rates in acute myocardial infarction. Ann Intern Med 2012; 156(9):618-26. doi: 10.7326/0003-4819-156-9-201205010-00003 [Crossref] [ Google Scholar]
- Kristensen SD, Laut KG, Fajadet J, Kaifoszova Z, Kala P, Di Mario C. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011: current status in 37 ESC countries. Eur Heart J 2014; 35(29):1957-70. doi: 10.1093/eurheartj/eht529 [Crossref] [ Google Scholar]
- Chandrashekhar Y, Alexander T, Mullasari A, Kumbhani DJ, Alam S, Alexanderson E. Resource and infrastructure-appropriate management of ST-segment elevation myocardial infarction in low- and middle-income countries. Circulation 2020; 141(24):2004-25. doi: 10.1161/circulationaha.119.041297 [Crossref] [ Google Scholar]
- Xu H, Yang Y, Wang C, Yang J, Li W, Zhang X. Association of hospital-level differences in care with outcomes among patients with acute ST-segment elevation myocardial infarction in China. JAMA Netw Open 2020; 3(10):e2021677. doi: 10.1001/jamanetworkopen.2020.21677 [Crossref] [ Google Scholar]
- Wilson PWF, D’Agostino RB Sr. No one size fits all: scoring risk of in-hospital death after myocardial infarctio. J Am Coll Cardiol 2016; 68(6):636-8. doi: 10.1016/j.jacc.2016.06.001 [Crossref] [ Google Scholar]
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018; 39(2):119-77. doi: 10.1093/eurheartj/ehx393 [Crossref] [ Google Scholar]
- Statistical Centre of Iran. Estimation of population in Iran by province and year. [Cited 1 Jan 2021]. Available from: https://www.amar.org.ir/english/Population-and-Housing-Censuses.
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 2018; 72(18):2231-64. doi: 10.1016/j.jacc.2018.08.1038 [Crossref] [ Google Scholar]
- Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA. TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation: an intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation 2000; 102(17):2031-7. doi: 10.1161/01.cir.102.17.2031 [Crossref] [ Google Scholar]
- Expert Panel on Detection, Evaluation Evaluation. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 2001; 285(19):2486-97. doi: 10.1001/jama.285.19.2486 [Crossref] [ Google Scholar]
- Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150(9):604-12. doi: 10.7326/0003-4819-150-9-200905050-00006 [Crossref] [ Google Scholar]
- 15 Greenland S, Pearce N. Statistical foundations for model-based adjustments. Annu Rev Public Health 2015; 36:89-108. doi: 10.1146/annurev-publhealth-031914-122559 [Crossref] [ Google Scholar]
- Huber K, Goldstein P, Danchin N, Fox KA, Welsh R, Granger CB. Enhancing the efficacy of delivering reperfusion therapy: a European and North American experience with ST-segment elevation myocardial infarction networks. Am Heart J 2013; 165(2):123-32. doi: 10.1016/j.ahj.2012.10.032 [Crossref] [ Google Scholar]
- Danchin N, Coste P, Ferrières J, Steg PG, Cottin Y, Blanchard D. Comparison of thrombolysis followed by broad use of percutaneous coronary intervention with primary percutaneous coronary intervention for ST-segment-elevation acute myocardial infarction: data from the French registry on acute ST-elevation myocardial infarction (FAST-MI). Circulation 2008; 118(3):268-76. doi: 10.1161/circulationaha.107.762765 [Crossref] [ Google Scholar]
- Victor SM, Subban V, Alexander T, G BC, Srinivas A, S S. A prospective, observational, multicentre study comparing tenecteplase facilitated PCI versus primary PCI in Indian patients with STEMI (STEPP-AMI). Open Heart 2014; 1(1):e000133. doi: 10.1136/openhrt-2014-000133 [Crossref] [ Google Scholar]
- McNamara RL, Kennedy KF, Cohen DJ, Diercks DB, Moscucci M, Ramee S. Predicting in-hospital mortality in patients with acute myocardial infarction. J Am Coll Cardiol 2016; 68(6):626-35. doi: 10.1016/j.jacc.2016.05.049 [Crossref] [ Google Scholar]
- Redfors B, Furer A, Selker HP, Thiele H, Patel MR, Chen S. Effect of smoking on outcomes of primary PCI in patients with STEMI. J Am Coll Cardiol 2020; 75(15):1743-54. doi: 10.1016/j.jacc.2020.02.045 [Crossref] [ Google Scholar]
- Yadav M, Mintz GS, Généreux P, Liu M, McAndrew T, Redfors B. The smoker’s paradox revisited: a patient-level pooled analysis of 18 randomized controlled trials. JACC Cardiovasc Interv 2019; 12(19):1941-50. doi: 10.1016/j.jcin.2019.06.034 [Crossref] [ Google Scholar]
- Gupta T, Kolte D, Khera S, Harikrishnan P, Mujib M, Aronow WS. Smoker’s paradox in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. J Am Heart Assoc 2016; 5(4):e003370. doi: 10.1161/jaha.116.003370 [Crossref] [ Google Scholar]
- Joner M, Cassese S. The “smoker’s paradox”: the closer you look, the less you see. JACC Cardiovasc Interv 2019; 12(19):1951-3. doi: 10.1016/j.jcin.2019.07.028 [Crossref] [ Google Scholar]
- Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017; 377(1):13-27. doi: 10.1056/NEJMoa1614362 [Crossref] [ Google Scholar]
- Ratwatte S, Hyun K, D’Souza M, Barraclough J, Chew DP, Shetty P. Relation of body mass index to outcomes in acute coronary syndrome. Am J Cardiol 2021; 138:11-9. doi: 10.1016/j.amjcard.2020.09.059 [Crossref] [ Google Scholar]
- Wang ZJ, Zhou YJ, Galper BZ, Gao F, Yeh RW, Mauri L. Association of body mass index with mortality and cardiovascular events for patients with coronary artery disease: a systematic review and meta-analysis. Heart 2015; 101(20):1631-8. doi: 10.1136/heartjnl-2014-307119 [Crossref] [ Google Scholar]
- Akin I, Tölg R, Hochadel M, Bergmann MW, Khattab AA, Schneider S. No evidence of “obesity paradox” after treatment with drug-eluting stents in a routine clinical practice: results from the prospective multicenter German DESDE (German Drug-Eluting Stent) Registry. JACC Cardiovasc Interv 2012; 5(2):162-9. doi: 10.1016/j.jcin.2011.09.021 [Crossref] [ Google Scholar]
- Nalini M, Sharafkhah M, Poustchi H, Sepanlou SG, Pourshams A, Radmard AR. Comparing anthropometric indicators of visceral and general adiposity as determinants of overall and cardiovascular mortality. Arch Iran Med 2019; 22(6):301-9. [ Google Scholar]
- Ahmadi A, Soori H, Mehrabi Y, Etemad K, Sajjadi H, Sadeghi M. Predictive factors of hospital mortality due to myocardial infarction: a multilevel analysis of Iran’s National Data. Int J Prev Med 2015; 6:112. doi: 10.4103/2008-7802.170026 [Crossref] [ Google Scholar]
- Saadatagah S, Ghodsi S, Omidi N, Poorhosseini H, Salarifar M, Sadeghian S. Twelve-year history of STEMI management in Tehran Heart Center: concomitant reduction of in-hospital mortality and hospitalization length. Arch Iran Med 2020; 23(8):514-21. doi: 10.34172/aim.2020.53 [Crossref] [ Google Scholar]