Arch Iran Med. 24(12):862-868.
doi: 10.34172/aim.2021.129
Original Article
Safety and Efficacy of Graded Gradual Pneumatic Balloon Dilation in Idiopathic Achalasia Patients: A 24-Year Single-Center Experience
Narges Fazlollahi 1  , Amir Anushiravani 1, Maryam Rahmati 2, Mohammad Amani 1, Hossein Asl-Soleimani 1, Melineh Markarian 1, Alice Chu Jiang 3, Javad Mikaeli 1, *
, Amir Anushiravani 1, Maryam Rahmati 2, Mohammad Amani 1, Hossein Asl-Soleimani 1, Melineh Markarian 1, Alice Chu Jiang 3, Javad Mikaeli 1, * 
Author information:
1Autoimmune and Motility Disorders Research Center, Digestive Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran
2Department of Epidemiology and Biostatistics, School of Public Health, Tehran University, Tehran, Iran
3Division of Digestive Diseases, Rush University Medical Center, Chicago, USA
*Corresponding Author: Javad Mikaeli, MD; Digestive Diseases Research Institute, Tehran University of Medical Sciences, Shariati Hospital, Karegar Shomali Ave., Tehran 14117-13135, Iran. Tel:+98-21-82415000; Fax:+98-21-82415400; Email:
mikaeli@ams.ac.ir
Abstract
Background:
Pneumatic balloon dilation (PBD) is a first line treatment for idiopathic achalasia. Here we report the safety and efficacy of graded gradual PBD on short and long-term follow-up.
Methods:
We evaluated 1370 idiopathic achalasia patients over a period of 24 years (1994-2018), prospectively. 216 patients did not undergo PBD due to comorbid diseases. Ultimately, 1092 achalasia patients were enrolled. All patients underwent graded gradual PBD, with repeat dilation if symptoms relapsed. Response to treatment was evaluated by Vantrappen scoring system.
Results:
Of 1092 achalasia patients, 937 patients were treated by PBD and 155 patients were treated by combined therapy (PBD 1 month after Botulinum toxin injection). In short-term follow-up, 728 of 1092 patients underwent one PBD and 77.3% of them had excellent or good response (responders), 163 patients (58.6%) who underwent two PBDs were responders, and 44 (51.2%) patients who underwent three PBDs were responders. Overall, 2193 balloon dilations were performed on 1092 patients (mean 2 PBDs/patient). Of 786 patients with long-term follow-up, 259 patients had excellent or good response with one PBD. The responders with two, three, and four or more dilations were 149, 67, and 67, respectively. The overall response rate was 69%. No any serious complications were noted by using the graded gradual method.
Conclusion:
Our results show that graded gradual PBD is a safe and effective method for treatment of achalasia patients, and achieves sufficient short and long-term symptomatic remission with high cumulative success rate.
Keywords: Achalasia, Efficacy, Pneumatic balloon dilation, Safety
Copyright and License Information
© 2021 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Fazlollahi N, Anushiravani A, Rahmati M, Amani M, Asl-Soleimani H, Markarian M, et al. Safety and efficacy of graded gradual pneumatic balloon dilation in idiopathic achalasia patients: a 24-year single-center experience. Arch Iran Med. 2021;24(12):862-868. doi: 10.34172/aim.2021.129
Introduction
Achalasia is an uncommon motility disorder of the esophagus influencing both sexes with equivalent occurrence and a prevalence of 0.5–1/10 000.1 It is usually diagnosed between the third and sixth decades of life,1,2 although it may occur at any age.
Aperistalsis and incomplete lower esophageal sphincter (LES) relaxation are the principal characteristics for achalasia.3 Therapeutic options for achalasia include endoscopic pneumatic balloon dilation (PBD),1 intrasphincteric botulinum toxin injections,4 ethanolamine oleate injections,5,6 peroral endoscopic myotomy, and surgical treatments such as minimally invasive laparoscopic or thoracoscopic cardiomyotomy.7-9 PBD has been a well-established treatment for many years, and is a relatively inexpensive outpatient procedure10 associated with high success rates ranging from 70% to 90%.11 Esophageal perforation is the most serious complication that occurs in about 2–4% of cases. High dilation pressures, balloon instability, repeated dilations in one session, high-amplitude contractions, longer duration of symptoms, age > 65 years, and presence of esophageal diverticula are considered risk factors for esophageal perforation in PBD.12-14 A graded balloon dilation technique has been shown to reduce the risk of perforation significantly.15 In our previous studies, after switching to the graded gradual method for balloon dilation, the risk of perforation was reduced to zero.16,17
Given the rarity of the disease, long-term data on the efficacy of PBD in a large series of achalasia patients are scarce. Here, we aimed to report the safety and efficacy of graded PBD technique in a large cohort of achalasia patients over long-term follow-up.
Materials and Methods
Patients
We prospectively enrolled 1370 adult patients with idiopathic achalasia referring to Shariati Hospital in Tehran over a period of 24 years from 1994 to 2018. Patients under 14 years of age were referred to the Pediatric Gastroenterology ward and were not included in this study. Two hundred sixteen patients with comorbid diseases and those who were poor candidates for PBD were treated by botulinum toxin or ethanolamine oleate injection and excluded from the study. In our first group of 62 patients in 1994, the initial session of PBD was performed with a 35mm balloon with perforations occurring in three patients.18 Therefore, we excluded our first 62 patients and enrolled a subsequent cohort of patients who underwent graded gradual PBD.
In total, 1092 achalasia patients participated in this study. Achalasia was diagnosed based on clinical presentation, radiographic features (timed barium esophagogram), and endoscopic and manometric findings.18 All patients signed the informed consent after a full discussion of risks, benefits, and alternatives of treatments. All patients underwent graded gradual PBD with repeat dilation performed in patients with symptom relapse. Patients who had rapid relapse, defined as less than 6 months after three sessions of PBD, and those who did not agree to surgery, underwent combined treatment of botulinum toxin injection and re-dilation after one month as described.19
Patients’ symptoms were scored according to the Achalasia Symptoms Score (ASS) (Tables 1 and 2). A questionnaire was completed including patient’s name, gender, age, telephone number, baseline symptoms and their duration and frequency, aggravating and alleviating factors of dysphagia, family history, medical history, timed barium esophagogram (TBE) findings, endoscopic and manometric findings, type of treatment sessions, and symptoms on follow-up. Baseline characteristics are reported in Table 3. Response to treatment was documented using the Vantrappen scoring system (Table 4).
Table 1.
Achalasia Symptoms Score
|
Symptom
|
Each meal
|
Daily
|
Weekly
|
None
|
| Dysphagia to solids |
3 |
2 |
1 |
0 |
| Dysphagia to liquids |
3 |
2 |
1 |
0 |
| Active regurgitation |
3 |
2 |
1 |
0 |
| Passive regurgitation |
3 |
2 |
1 |
0 |
| Chest pain |
3 |
2 |
1 |
0 |
Table 2.
Severity Score of Dysphagia for Every Swallow
|
Severity
|
Score
|
Description
|
| No dysphagia |
0 |
Normal passage of food from LES zone. |
| Mild dysphagia |
1 |
Sensation or short delay of passage of food from LES, without need for water. |
| Moderate dysphagia |
2 |
Need for water for passage of food from LES zone. |
| Severe dysphagia |
3 |
Accompanied by passive or active regurgitation. |
Table 3.
Baseline Characteristics of the Study Population
|
Characteristics
|
Mean±SD
|
| Age (y) |
38.4 ± 15 |
| Sex (M/F) |
547/545 |
| Duration of symptoms before diagnosis (year) |
4.2 ± 4.6 |
| Initial symptom score |
10.1 ± 3.2 |
| Initial LES pressure (mm Hg) |
39.7 ± 23.8 (n = 662) |
LES, lower esophageal sphincter.
Table 4.
Vantrappen Scoring System
|
Class
|
Dysphagia
|
| Excellent |
Completely free of symptoms. |
| Good |
Occasional (less than once a week) dysphagia or pain of short duration defined as retrosternal hesitation of food lasting from 2–3 s to 2–3 min and disappearing after drinking fluids. |
| Moderate |
Dysphagia more than once a week lasting less than 2–3 min and not accompanied by regurgitation or weight loss. |
| Poor |
Dysphagia more than once a week or lasting 2–3 min or longer or accompanied by regurgitation or weight loss. |
Symptom scores were assessed by a physician (MD), and all of the PBDs were performed under supervision of one gastroenterologist who is experienced in PBD (J.M).5,6,16,17,20,21
Pneumatic Balloon Dilation
PBDs were performed using a Rigiflex balloon (Boston Scientific Corporation, Natick, MA), with a graded scale under direct endoscopic visualization. Conscious sedation was given using intravenous meperidine (25–50 mg) and diazepam (5–10 mg) after a clear liquid diet for 24h and an overnight fast. After 2015, PBDs were performed with deep sedation using fentanyl (1–2 µg/kg), midazolam (0.05 mg/kg), and propofol 20 mg bolus with 0.025–0.075 mg/kg/min infusion by an anesthesiologist. Following a complete esophagogastroduodenoscopy, a 0.035 mm guide wire was placed in the antrum and a balloon dilator was passed over it. The center of the Rigiflex balloon was placed at the gastroesophageal junction under video endoscopic guidance.
The 30 mm balloon was inflated from 3 psi with increase in 3 psi every 10 seconds up to 15 psi over 40 seconds and maintained for another 60 seconds. After deflation of the balloon and advancement into the stomach, the gastroesophageal junction was reassessed endoscopically for any evidence of severe bleeding or perforation. Mild oozing of blood was an expected finding after balloon dilation due to mucosal disruption. The patients were discharged after 3 hours of observation. If tachycardia or persistent chest pain developed post-procedure, a gastrografin swallow was completed to rule out perforation.
In the follow-up period, patients who had relapse of symptoms underwent TBE and if barium retention was noted at 5 minutes, re-dilation was performed. In the case of symptomatic relapse but normal timed esophagogram, TBE was repeated after 3 months and if objective (radiographic) relapse was confirmed, retreatment was recommended. For these patients, the graded PBD method was applied by performing balloon dilation to 35 mm for the first relapse. For patients with a second relapse, we performed balloon dilation to 35 mm if the relapse occurred after more than 6 months from the second PBD and to 40 mm if the relapse occurred less than 6 months after the second PBD. In 50 patients whose symptoms relapsed more than 1 year after the last PBD and with tight LES on endoscopy, we repeated balloon dilation to 30 mm.
Symptomatic Response
The questionnaire included clinical data such as the achalasia symptom score (ASS) similar to our previous studies.5,6,9,16 The severity of each symptom was recorded on a scale of 0 to 3, depending on its frequency. The five cardinal symptoms scores were added to the severity score of dysphagia (Tables 1 and 2), summing to a maximum score of 18. Good clinical response was defined as a decrease in ASS to 4 or less, and absence of regurgitation or severe dysphagia. Clinical relapse was considered if the severity score of dysphagia had an increase of 2 or more points after an initial good clinical response. We considered a patient in a sustained good response if they remained in clinical remission (ASS ≤ 4) one year after treatment and at follow-up intervals. The patients were followed by clinic visits or phone interview every 6 months and at the end of follow-up. Patients were told to refer for re-evaluation if they had severe dysphagia or regurgitation.
At the end of follow-up, the Vantrappen score was used for evaluation of response to treatment and classified as follows: excellent, good, moderate, and poor. Patients with excellent or good responses were considered responders to treatment.11
Out of 1092 patients, 786 (72%) were followed for more than 1 year. No perforation or any serious complications such as severe bleeding or intramural hematoma occurred using the graded gradual method.
Thirty-four of the 1092 patients (3.1%) were observed in the hospital more than 3 hours following PBD due to persistent or recurrent pain. Chest x-ray, gastrografin swallow, and CT scan of the chest showed no incidences of perforation in these patients, and they were discharged from the hospital within 24 hours.
Statistical Analysis
Continuous variables were reported as mean ± standard deviation or median (interquartile range). Categorical variables were reported as frequency (percentage). The mean ASS of patients was compared between baseline and follow-up using paired sample t-test.
In order to explore the impact of important risk factors on survival time in long-term follow-up, a Cox proportional hazards model was used. The time between treatment initiation and the last follow-up was considered as survival time. Changes in phone numbers or addresses, death, or noncompliance were the most common reasons for loss to follow-up and were considered as censored, and non-responders were considered as an event. Hazard ratios (HRs) were obtained for potential risk factors. Variables with P value < 0.2 were entered in a multiple Cox model. Using a stepwise model, non-significant variables were excluded and significant risk factors were found. We checked proportionality by including time-dependent covariates in the model.
Statistical analysis was performed using STATA (version 14; STATA Inc., College station, TX, USA), with P < 0.05 and confidence interval at 95% considered as significant.
Results
Of the 1092 achalasia patients included in this study during the 24-year study period, 547 (50.1%) were men and 545 (49.9%) were women. The mean ± SD age of our patients was 38.4 ± 15 years. The mean ± SD duration of symptoms before diagnosis was 4.2 ± 4.6 years. The prevalence of symptoms related to achalasia is shown in Figure 1; the most common were dysphagia to solids and liquids at 98.8% and 87.6%, respectively. Aggravating and alleviating factors of dysphagia are listed in Table 5.
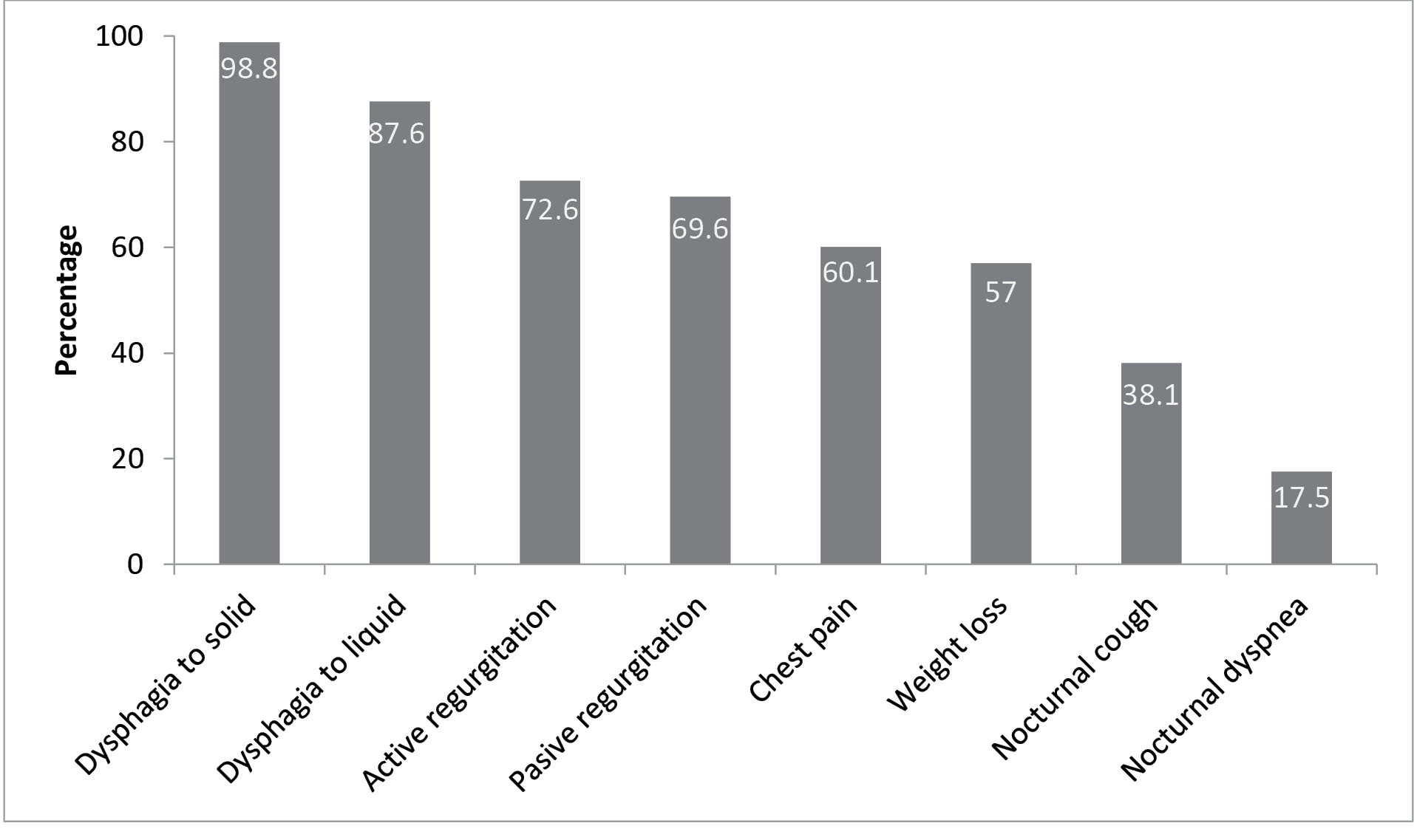
Figure 1.
Frequency of Achalasia Symptoms.
.
Frequency of Achalasia Symptoms.
Table 5.
Aggravating and Alleviating Factors of Dysphagia
|
Aggravating factors
|
| • |
Only during stressful eating |
10.1% |
| • |
Only during hurried eating |
25.5% |
| • |
Both during stressful and hurried eating |
69.5% |
|
Alleviating factors
|
| • |
Water drinking |
69.6% |
| • |
Back straightening |
34.6% |
| • |
Standing & walking |
25.8% |
| • |
Deep breathing |
7.2% |
| • |
Valsalva maneuver |
6.7% |
| • |
Massage on sternum |
6.5% |
The mean ± SD LES pressure before treatment in 662 patients with available manometry data was 39.7 ± 23.8 mm Hg. The mean ASS of patients decreased from 10.1 ± 3.2 before treatment to 4.90 ± 4.7 at 1 year after treatment (P < 0.001) and 2.9 ± 3.1 at the final follow-up (P < 0.001).
Of the 1092 patients, 937 (85.8%) were treated by PBD only. One hundred fifty-five (14.2%) patients were treated by combined therapy. In total, 2193 balloon dilations were done for 1092 patients with an average of 2 balloons per patient. Of these dilations, 1142 balloons were dilated to 30 mm, 944 balloons were dilated to 35 mm and 107 balloons were dilated to 40 mm. No perforation or any serious complications such as severe bleeding occurred using the graded gradual method.
Short-term Outcomes of Pneumatic Balloon Dilation
The Vantrappen achalasia questionnaire was used to evaluate treatment efficacy. All patients were followed and response to treatment was assessed at 1 year after first PBD. Of the 1092 patients, 728 (66.7%) had only 1 dilation, while 278 (25.5%) had 2 dilations and 86 (7.8%) had 3 dilations as primary therapy during the first 12 months from initiation of therapy.
Of 728 patients with one PBD, 563 (77.3%) had excellent or good response. Of 278 and 86 patients with second or third PBD, 163 (58.6%) and 44 (51.2%) had excellent or good responses, respectively according to Vantrappen scoring (Table 6).
Table 6 shows the number of PBDs and Vantrappen score at 1 year after treatment according to sex. Out of 361 women with one PBD, 277 (76.7%) were responders defined by an excellent or good response on Vantrappen score; of 367 men who underwent one PBD, 286 (77.9%) were responders. Men and women were not different when comparing the number of successful (P = 0.6) or failed PBDs (P = 0.7).
Table 6.
Number of PBD and Vantrappen Score at 1 Year After Treatment According to Sex (Excellent or Good Scores Defined as Responder, Moderate or Poor Scores Defined as Non-responder)
|
Times
|
Male
|
Female
|
Total
|
|
Responders
|
Non-responders
|
Responders
|
Non-responders
|
Responders
|
Non-responders
|
| 1 |
286 (77.9) |
81 (22.1) |
277 (76.7) |
84 (23.3) |
563 (77.3) |
165 (22.7) |
| 2 |
80 (62) |
49 (38) |
83 (55.7) |
66 (44.3) |
163 (58.6) |
115 (41.4) |
| ≥ 3 |
24 (47) |
27 (53) |
20 (57.1) |
15 (42.9) |
44 (51.2) |
42 (48.8) |
| Total |
390 (71.3) |
157 (28.7) |
380 (69.7) |
165 (30.3) |
770 (70.5) |
322 (29.5) |
The median (IQR) time between the first (dilation to 30 mm) and second PBD (dilation to 35 mm) was 3.9 (2.3–6.6) months, and between the second (dilation to 35 mm) and third (dilation to 40 mm) PBD was 3.7 (2.5–5.7) months.
Long-term Outcomes of Pneumatic Balloon Dilation
Seven hundred eighty-six patients were followed for more than one year, with a median follow-up of 8.8 years (IQR: 6.4–16.9 years). Response to treatment was excellent in 269 (34.2%), good in 273 (34.7%), moderate in 156 (19.8%) and poor in 88 (11.2%). Overall, 69% (542 cases) were considered responders to treatment (Table 7). Of the responders, PBD was performed once in 47.8% (n = 259) of patients, twice in 27.5% (n = 149), three times in 12.4% (n = 67), and four or more times in 12.2% (n = 67) over 24 years of follow-up. Patients in the moderate response group, according to Vantrappen score, did not have severe dysphagia, regurgitation, or weight loss. They often tolerated their symptoms and did not seek more aggressive therapeutic options such as surgery. On long-term follow-up of 357 patients who underwent one dilation, 98 (27.5%) patients were non-responders, and of 228 patients with two dilations, 34.7% of patients were non-responders. Of 105 patients with three dilations, 38 (36.2%) patients were non-responders, and of 96 patients who underwent four or more dilations, 29 (30.2%) patients were non-responders (Table 7). At the end of follow-up, 49 (6.2%) patients were referred for cardiomyotomy due to multiple relapses and resistance to PBD. There was significant difference between the number of responders and non-responders in patients who underwent one PBD compared to multiple PBDs (P < 0.001).
Table 7.
Number of PBD and Vantrappen Score at Final follow Follow-up by Sex (Excellent or Good Scores Defined as Responder, Moderate or Poor Scores Defined as Non-responder).
|
Times
|
Male
|
Female
|
Total
|
|
Responders
|
Non-responders
|
Responders
|
Non-responders
|
Responders
|
Non-responders
|
| 1 |
128 (73.14) |
47 (26.86) |
131 (71.98) |
51 (28.02) |
259 (72.5) |
98 (27.5) |
| 2 |
76 (67.86) |
36 (32.14) |
73 (62.93) |
43 (37.07) |
149 (65.3) |
79 (34.7) |
| 3 |
37 (64.91) |
20 (35.09) |
30 (62.5) |
18 (37.5) |
67 (63.8) |
38 (36.2) |
| ≥ 4 |
32 (66.67) |
16 (33.33) |
35 (72.92) |
13 (27.08) |
67 (69.8) |
29 (30.2) |
| Total |
273 (69.64) |
119 (30.36) |
269 (68.27) |
125 (31.73) |
542 (68.9) |
244 (31.1) |
The median duration of remission with good or excellent response was 6.9 years (IQR: 4.7–15) for one PBD, 6.2 years (IQR: 3.9–11.6) for two PBDs, and 4.7 years (2.3–8.5) for three PBDs.
There was no significant difference in follow-up time between patients with successful versus failed PBDs (P = 0.4).
Predictors of Response
Factors such as age, first symptoms, total symptom score at baseline, manometric findings (LES pressure and type of achalasia) and TBE (height and volume of the barium at 5min) were assessed as predicting factors for response to PBD at one year after first PBD. Patients with lower baseline symptom score (P = 0.005, Adjusted HR (95% CI): 1.09 (1.02–1.15)), higher baseline LES pressure (P < 0.001, Adjusted HR (95% CI): 0.98 (0.97–0.99)), and a family history of achalasia had better response to the treatment (p = 0.006, Adjusted HR (95% CI) = 2.10 (1.24–3.57) (Table 8). Other factors did not have an effect on rates of clinical response.
Table 8.
Predictors of Response to Therapy Using Multiple Cox Model (N at analysis = 414)
|
|
Adjusted HR (95% CI)
|
P
Value
|
| Total symptom score |
1.09 (1.02–1.15) |
0.005 |
| LES pressure |
0.98 (0.97–0.99) |
< 0.001 |
| Family history of achalasia |
2.10 (1.24–3.57) |
0.006 |
LES, lower esophageal sphincter.
Discussion
PBD is recommended as a first line treatment choice to obtain long-term responsiveness.22 Some studies found that surgical myotomy had better long-term clinical response than PBD,23 while others reported similar efficacy or superiority of PBD.24-26 A randomized controlled trial by Kostic et al found that laparoscopic myotomy had potential superiority over PBD after 12 months of follow-up.25 In another randomized trial comparing laparoscopic Heller myotomy (LHM) with PBD by Boeckxstaens et al, the rate of treatment success was similar at 90% with LHM and 86% with PBD after 2 years. Esophageal emptying as measured by the height of barium-contrast column, LES pressure, and quality of life were also similar between the two groups.24
The European achalasia trial compared the long-term response of PBD and LHM showing similar success rates after five years – 82% and 84%, respectively.27 However, 25% of PBD patients required repeat dilation during follow-up. Lynch et alstudied 463 patients with achalasia who had PBD or LHM, and concluded that in the hands of experienced operators, PBD was safer and had a lower mortality rate.28
In this study, we report our experience with a large cohort of achalasia patients who were treated by graded gradual PBD technique over 24 years of the study period. Patients were assessed and treated by a single physician (J.M.). We showed that PBD is an effective and safe procedure with an overall response rate of 69%. Long-term single-center data on efficacy of PBD is scarce.
We have shown that according to the Vantrappen criteria, one PBD alone led to treatment success in short-term follow-up at one year in 77.3% patients, which is in line with previous studies.22,29,30 However, in the long-term (more than one year), the success rate of one session of PBD declined to 33%. This is similar to studies with long-term follow-up reporting a success rate of 30% to 40%.31,32 We came across different protocols for PBD in achalasia patients while reviewing the literature.22 The success rates of endoscopic management of achalasia vary according to the criteria used to define clinical response and heterogeneities in technical approaches. The present study defined treatment success using the Vantrappen system score.
Our study found that on long-term follow-up of more than 1 year, 33% of patients were responders after a single PBD with 30mm balloon, a cumulative 52% of patients were responders with second dilation. At the end of follow-up with repeated dilations, we achieved an overall response rate of 69%. In agreement with our results, previous studies have demonstrated that the need for re-dilation in case of recurrent symptoms after PBD increases treatment success rates.33 Longer remission of symptoms was not seen in those with subsequent PBDs.30,34 While a few studies have shown that other treatments such as surgery maintain remission for a longer period of time,35 others report achieving long-term remission with PBD.30,34
In our study, more than half of the patients who underwent subsequent PBDs after the second dilation had a durable response at 1 year after treatment. While some studies suggest a lower likelihood of sustained remission after two failed dilations,6,20 our data suggest that surgery could be reserved for patients with more unsuccessful pneumatic dilations. Among patients with unsuccessful frequent PBDs (> 3 sessions within 1 year and ASS of more than 4 at 1 year after treatment), the majority declined surgery and underwent a protocol of combined treatment with botulinum toxin injection followed by PBD after one month. Of these patients, 77% had durable response for 1 year (17) and it may be therefore suggested as an approach in such patients.11,17,33
In a prior study, there was no significant difference in baseline LES pressure between successful or failed treatment.35 A higher LES pressure was shown to be a possible predictor of symptom recurrence after PBD.32 However, in our study, patients with higher LES pressure at baseline had better response to treatment. Eckart and colleagues concluded that the balloon size could predict a successful result after one session of PBD32; however, the present study did not find a higher chance of re-dilation when we used a small balloon.
A major complication of PBD is esophageal perforation. Some studies report esophageal perforation rates in the range of 1–2%24,25,28,30 and others report a range of 2–4%.19,27,29,31 However, in our study, no esophageal perforation was seen in 2193 PBDs in 1092 achalasia patients with a graded gradual dilation method. In our approach to PBD, we positioned the balloon under direct videoendoscopic visualization, which compared to PBD under fluoroscopy, is simpler and less costly, and is still associated with an acceptable efficacy and high safety.11,17,33
The strength of our study is that it presents long-term data from a large cohort of achalasia patients treated with graded gradual PBD as their first therapy in a single referral center with no major complications. However, our study has some limitations. First, we did not assess the rate of gastroesophageal reflux (GER) after PBD with 24 h pH metry. It is difficult to distinguish GER from achalasia because of the similarity of symptoms such as heartburn, chest pain and dysphagia in both conditions. In our database, only 31 patients who underwent endoscopy because of symptomatic relapse had erosive GER. Second, some patients were lost in long-term follow-up due to change in contact information. We reduced this limitation by asking for more than one contact number or sending a letter to their address.
In conclusion, our results show that graded gradual PBD is an effective and safe method for treatment of achalasia patients, and achieves sufficient short- and long-term symptomatic remission with a high cumulative success rate.
Authors’ Contribution
JM and HAS designed the study. Patients were treated by AA, MA, and JM. MR did the statistical analysis. NF and AA wrote the article. Data gathering was done by NF and MM. All authors read and approved the final version of the article.
Conflict of Interest Disclosures
All authors declared no conflicts of interest.
Ethical Statement
The Ethics Committee for Medical Research at DDRI reviewed and approved the study.
References
- Rai RR, Shende A, Joshi A, Mathur A, Nijhawan S. Rigiflex pneumatic dilation of achalasia without fluoroscopy: a novel office procedure. Gastrointest Endosc 2005; 62(3):427-31. doi: 10.1016/j.gie.2005.04.008 [Crossref] [ Google Scholar]
- Emami MH, Raisi M, Amini J, Daghaghzadeh H. Achalasia and thyroid disease. World J Gastroenterol 2007; 13(4):594-9. doi: 10.3748/wjg.v13.i4.594 [Crossref] [ Google Scholar]
- Borotto E, Gaudric M, Danel B, Samama J, Quartier G, Chaussade S. Risk factors of oesophageal perforation during pneumatic dilatation for achalasia. Gut 1996; 39(1):9-12. doi: 10.1136/gut.39.1.9 [Crossref] [ Google Scholar]
- Muehldorfer SM, Schneider TH, Hochberger J, Martus P, Hahn EG, Ell C. Esophageal achalasia: intrasphincteric injection of botulinum toxin A versus balloon dilation. Endoscopy 1999; 31(7):517-21. doi: 10.1055/s-1999-56 [Crossref] [ Google Scholar]
- Niknam R, Mikaeli J, Mehrabi N, Mahmoudi L, Elahi E, Shirani S. Ethanolamine oleate in resistant idiopathic achalasia: a novel therapy. Eur J Gastroenterol Hepatol 2011; 23(12):1111-5. doi: 10.1097/MEG.0b013e328349647e [Crossref] [ Google Scholar]
- Niknam R, Mikaeli J, Fazlollahi N, Mahmoudi L, Mehrabi N, Shirani S. Ethanolamine oleate as a novel therapy is effective in resistant idiopathic achalasia. Dis Esophagus 2014; 27(7):611-6. doi: 10.1111/dote.12122 [Crossref] [ Google Scholar]
- Kiudelis M, Mickevicius A, Maleckas A, Endzinas Z, Kiudelis G, Jonaitis L. Laparoscopic myotomy or pneumatic dilatation for achalasia treatment?. Cent Eur J Med 2011; 6(5):640. doi: 10.2478/s11536-011-0072-7 [Crossref] [ Google Scholar]
- Abu Gazala M, Khalaila A, Shussman N, Abu Gazala S, Elazary R, Amar D. Transesophageal endoscopic myotomy for achalasia: recognizing potential pitfalls before clinical application. Surg Endosc 2012; 26(3):681-7. doi: 10.1007/s00464-011-1937-1 [Crossref] [ Google Scholar]
- Amani M, Fazlollahi N, Shirani S, Malekzadeh R, Mikaeli J. Assessment of pneumatic balloon dilation in patients with symptomatic relapse after failed Heller myotomy: a single center experience. Middle East J Dig Dis 2016; 8(1):57-62. doi: 10.15171/mejdd.2016.08 [Crossref] [ Google Scholar]
- Tuset JA, Luján M, Huguet JM, Canelles P, Medina E. Endoscopic pneumatic balloon dilation in primary achalasia: predictive factors, complications, and long-term follow-up. Dis Esophagus 2009; 22(1):74-9. doi: 10.1111/j.1442-2050.2008.00874.x [Crossref] [ Google Scholar]
- Katsinelos P, Kountouras J, Paroutoglou G, Beltsis A, Zavos C, Papaziogas B. Long-term results of pneumatic dilation for achalasia: a 15 years’ experience. World J Gastroenterol 2005; 11(36):5701-5. doi: 10.3748/wjg.v11.i36.5701 [Crossref] [ Google Scholar]
- Nabi Z, Reddy DN. Achalasia cardia–recent advances in diagnosis and endoscopic management. J Gastrointest Dig Syst 2016; 6(6):393. doi: 10.4172/2161-069x.1000393 [Crossref] [ Google Scholar]
- Vanuytsel T, Lerut T, Coosemans W, Vanbeckevoort D, Blondeau K, Boeckxstaens G. Conservative management of esophageal perforations during pneumatic dilation for idiopathic esophageal achalasia. Clin Gastroenterol Hepatol 2012; 10(2):142-9. doi: 10.1016/j.cgh.2011.10.032 [Crossref] [ Google Scholar]
- Katzka DA, Castell DO. Review article: an analysis of the efficacy, perforation rates and methods used in pneumatic dilation for achalasia. Aliment Pharmacol Ther 2011; 34(8):832-9. doi: 10.1111/j.1365-2036.2011.04816.x [Crossref] [ Google Scholar]
- Pandolfino JE, Kahrilas PJ. Presentation, diagnosis, and management of achalasia. Clin Gastroenterol Hepatol 2013; 11(8):887-97. doi: 10.1016/j.cgh.2013.01.032 [Crossref] [ Google Scholar]
- Hasanzadeh A, Mikaeli J, Elahi E, Mehrabi N, Etemadi A, Malekzadeh R. Demographic, clinical features and treatment outcomes in 700 achalasia patients in iran. Middle East J Dig Dis 2010; 2(2):91-6. [ Google Scholar]
- Mikaeli J, Bishehsari F, Montazeri G, Mahdavinia M, Yaghoobi M, Darvish-Moghadam S. Injection of botulinum toxin before pneumatic dilatation in achalasia treatment: a randomized-controlled trial. Aliment Pharmacol Ther 2006; 24(6):983-9. doi: 10.1111/j.1365-2036.2006.03083.x [Crossref] [ Google Scholar]
- Mikaeli J, Bishehsari F, Montazeri G, Yaghoobi M, Malekzadeh R. Pneumatic balloon dilatation in achalasia: a prospective comparison of safety and efficacy with different balloon diameters. Aliment Pharmacol Ther 2004; 20(4):431-6. doi: 10.1111/j.1365-2036.2004.02080.x [Crossref] [ Google Scholar]
- Mikaeli J, Yaghoobi M, Montazeri G, Ansari R, Bishehsari F, Malekzadeh R. Efficacy of botulinum toxin injection before pneumatic dilatation in patients with idiopathic achalasia. Dis Esophagus 2004; 17(3):213-7. doi: 10.1111/j.1442-2050.2004.00410.x [Crossref] [ Google Scholar]
- Mikaeli J, Fazel A, Montazeri G, Yaghoobi M, Malekzadeh R. Randomized controlled trial comparing botulinum toxin injection to pneumatic dilatation for the treatment of achalasia. Aliment Pharmacol Ther 2001; 15(9):1389-96. doi: 10.1046/j.1365-2036.2001.01065.x [Crossref] [ Google Scholar]
- Mikaeli J, Yaghoobi M, Sohrabi MR, Malekzadeh R. Rigiflex balloon dilation without fluoroscopy for treatment of achalasia: A long-term follow-up of 99 patients. Acta Med Iran 2002; 40(2):69-72. [ Google Scholar]
- Hulselmans M, Vanuytsel T, Degreef T, Sifrim D, Coosemans W, Lerut T. Long-term outcome of pneumatic dilation in the treatment of achalasia. Clin Gastroenterol Hepatol 2010; 8(1):30-5. doi: 10.1016/j.cgh.2009.09.020 [Crossref] [ Google Scholar]
- Csendes A, Velasco N, Braghetto I, Henriquez A. A prospective randomized study comparing forceful dilatation and esophagomyotomy in patients with achalasia of the esophagus. Gastroenterology 1981; 80(4):789-95. [ Google Scholar]
- Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 2011; 364(19):1807-16. doi: 10.1056/NEJMoa1010502 [Crossref] [ Google Scholar]
- Kostic S, Kjellin A, Ruth M, Lönroth H, Johnsson E, Andersson M. Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia Results of a randomized controlled trial. World J Surg 2007; 31(3):470-8. doi: 10.1007/s00268-006-0600-9 [Crossref] [ Google Scholar]
- Vela MF, Richter JE, Khandwala F, Blackstone EH, Wachsberger D, Baker ME. The long-term efficacy of pneumatic dilatation and Heller myotomy for the treatment of achalasia. Clin Gastroenterol Hepatol 2006; 4(5):580-7. doi: 10.1016/s1542-3565(05)00986-9 [Crossref] [ Google Scholar]
- Moonen A, Annese V, Belmans A, Bredenoord AJ, Bruley des Varannes S, Costantini M. Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 2016; 65(5):732-9. doi: 10.1136/gutjnl-2015-310602 [Crossref] [ Google Scholar]
- Lynch KL, Pandolfino JE, Howden CW, Kahrilas PJ. Major complications of pneumatic dilation and Heller myotomy for achalasia: single-center experience and systematic review of the literature. Am J Gastroenterol 2012; 107(12):1817-25. doi: 10.1038/ajg.2012.332 [Crossref] [ Google Scholar]
- Karamanolis G, Sgouros S, Karatzias G, Papadopoulou E, Vasiliadis K, Stefanidis G. Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol 2005; 100(2):270-4. doi: 10.1111/j.1572-0241.2005.40093.x [Crossref] [ Google Scholar]
- Elliott TR, Wu PI, Fuentealba S, Szczesniak M, de Carle DJ, Cook IJ. Long-term outcome following pneumatic dilatation as initial therapy for idiopathic achalasia: an 18-year single-centre experience. Aliment Pharmacol Ther 2013; 37(12):1210-9. doi: 10.1111/apt.12331 [Crossref] [ Google Scholar]
- Vaezi MF, Baker ME, Achkar E, Richter JE. Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut 2002; 50(6):765-70. doi: 10.1136/gut.50.6.765 [Crossref] [ Google Scholar]
- Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: late results of a prospective follow up investigation. Gut 2004; 53(5):629-33. doi: 10.1136/gut.2003.029298 [Crossref] [ Google Scholar]
- Rohof WO, Boeckxstaens GE. Treatment of the patient with achalasia. Curr Opin Gastroenterol 2012; 28(4):389-94. doi: 10.1097/MOG.0b013e328353af8f [Crossref] [ Google Scholar]
- Zerbib F, Thétiot V, Richy F, Benajah DA, Message L, Lamouliatte H. Repeated pneumatic dilations as long-term maintenance therapy for esophageal achalasia. Am J Gastroenterol 2006; 101(4):692-7. doi: 10.1111/j.1572-0241.2006.00385.x [Crossref] [ Google Scholar]
- Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 2009; 249(1):45-57. doi: 10.1097/SLA.0b013e31818e43ab [Crossref] [ Google Scholar]