Arch Iran Med. 24(9):665-669.
doi: 10.34172/aim.2021.95
Original Article
Colectomy in Ulcerative Colitis: Trends in Southern Iran in a Decade
Sulmaz Ghahramani 1  , Mahsa Paparisabet 2, Mohammad Sayari 1, Seyed Vahid Hosseini 3, Kamran Bagheri Lankarani 1, *
, Mahsa Paparisabet 2, Mohammad Sayari 1, Seyed Vahid Hosseini 3, Kamran Bagheri Lankarani 1, * 
Author information:
1Health Policy Research Center, Institute of Health, Shiraz University of Medical Sciences, Shiraz, Iran
2Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran
3Colorectal Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
*Corresponding Author: Kamran Bagheri Lankarani, MD; Health Policy Research Center, Institute of Health, Shiraz University of Medical Sciences, Shiraz, Iran. Tel: +98-71-32309615; Fax: +98-71-32309615; Email:
kblankarani@yahoo.com
Abstract
Background:
Colectomy is considered as a part of therapeutic armamentarium in ulcerative colitis. The availability of new biologic treatments might have affected the trend of using this modality.
Methods:
The hospital records of all tertiary centers in Shiraz, which are the main centers for the treatment of ulcerative colitis (UC) in southern Iran, were reviewed to estimate the total number of admissions for the treatment of severe UC and colectomy among patients from 2009 to 2019. In this historical cohort study, information about the current status of the patients was collected by phone calls during December 2019.
Results:
Totally, 111 (4%) UC patients, out of 2933 admissions, underwent colectomy. Sixty-five (54.6%) UC colectomy patients were female. The results revealed an upward trend for the ratio of the frequency of colectomies to total UC admissions (Z = 3.39, P < 0.001). Colectomy complications occurred in 44 patients (40%), and most of the patients 38 (34%) had late complications, leading to readmission. Seven patients (6.3%) had died from colectomy during the follow-up calls. Most of the dead patients underwent urgent surgery and were young.
Conclusion:
Despite the use of biologics during the past decade in southern Iran, there was a rising trend among the UC patients’ colectomies. The frequencies of post-operative complications and mortality was considerable, highlighting the need for refinement of UC care in this region.
Keywords: Colectomy, Iran, Ulcerative colitis
Copyright and License Information
© 2021 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Ghahramani S, Paparisabet M, Sayari M, Hosseini SV, Bagheri Lankarani K. Colectomy in ulcerative colitis: trends in southern iran in a decade. Arch Iran Med. 2021;24(9):665-669. doi: 10.34172/aim.2021.95
Introduction
Inflammatory bowel diseases (IBDs) are chronic diseases affecting the gastrointestinal tract (GIT), especially the colon, through dysregulated immunity. They consist of two major categories, namely ulcerative colitis (UC) and Crohn’s disease (CD).1,2 Many Asian countries, including Iran, have witnessed a rise in the incidence of IBD.3 Studies in southern Iran revealed a dramatic increase in the incidence of UC over the past decades.4 IBD is a chronic disease, and most of the affected patients are young and need long-term care. In this regard, surgery is an attractive one-time treatment to avoid the chronic use of drugs; however, it may have several important side effects. UC differs from CD as it is a mucosal disease confined to the colon, compared to transmural involvement in CD which may occur at any location in the GIT from mouth to anus. This makes colectomy a more viable option in the treatment of UC in comparison to CD.2 The rate of colectomy varies worldwide. In Asia, the colectomy rate varies from 4% in the first year of diagnosis to more than 20% after 10 years.3
Colectomy is not free from complications, including the possibility of death.5-9 The total rate of mortality from colectomy among the UC patients is estimated to be about 3%.10
The advent of new therapeutics, including biologics and immunosuppressive treatment, has expanded the therapeutic armamentarium in UC. Recent reports indicate that lower colectomy rates are probably caused by the availability of these more effective drugs.11 There is no study on the effect of access to these therapies on UC colectomy in Iran.
This study aimed to examine the trend of UC colectomy over the past decade, particularly when anti-tissue necrosis factor (anti-TNF) biologics became widely available in Iran.
Materials and Methods
In this historical cohort study, we evaluated all adult patients (age ≥ 18 year), who were affected by UC and received colectomy in Shiraz during March 2009 to March 2019. All six hospitals located in Shiraz, Fars province, southern Iran, which offered colectomy for UC patients were included in this study as they are the centers providing UC patients with care services in southern Iran.
The UC diagnosis was confirmed on the basis of clinical, endoscopic, and histological criteria, as described elsewhere.12
The data in this study were collected by reviewing the hospital records using relevant ICD-10 codes. All the included patients underwent total proctocolectomy with end ileostomy or with ileal pouch anal anastomosis. In this regard, the patients with segmental colectomies and incomplete records were excluded.
The patients’ hospitalization data were recorded based on the discharge time prescribed by physicians or the time of death certificate among the hospitalized patients.
Furthermore, data on the patients’ readmission, including admission for colectomy complications, were also collected. The colectomy complications were categorized as early versus late. Early complications were defined as complications detected during the same admission period for colectomy or within four weeks of surgery, and the late complications were defined as complications diagnosed in subsequent admissions at least four weeks apart.
We contacted the patients via phone calls and interviewed them or their closest relatives regarding their current health status and any possible further complications. We also collected the data from all the UC patients admitted in the same hospitals during this period.
Statistical Methods and Data Analysis
Descriptive statistics were used to demonstrate mean and standard deviation (SD) for quantitative data, and frequency (percentage) was also used to describe qualitative information in the SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA). Significance level was set at 0.05. In survival analysis, event was described as “death after colectomy” due to a cause related to surgery, its complication or the disease process. Time to event was identified as “duration from colectomy to death (months)”. To estimate the rate of survival during each period, the Kaplan-Meier model and log rank test were used to compare two or more survival curves with the null hypothesis of a common survival curve. The Mann-Kendall trend test was used to identify the upward or downward trend, if any, of the colectomy frequencies and the total UC admissions.
Results
From March 2009 to March 2019, 111 (4%) UC patients, out of 2933 admissions, underwent colectomy. Sixty-five (54.6%) patients were female. The mean ± standard deviation (SD) of colectomy time after the first diagnosis of UC was 9.8 ± 7.2 years. Moreover, 71 (64.0%) patients had pancolitis. The characteristics of the patients who underwent colectomy are described in Table 1.
Table 1.
Characteristics of Ulcerative Colitis Patients Undergoing Colectomy.
|
Feature
|
|
N/Mean
|
%/Standard Deviation (Range)
|
| Age at colectomy (y) |
|
39.1 |
12.1 (16–77) |
| Age at definite diagnosis time (y) |
|
29.7 |
12.3 (6–64) |
| Gender |
Male |
51 |
45.9 |
| Female |
60 |
54.1 |
| Length of hospital stay (days) |
|
9.1 |
6.1 (3–45) |
| Marital status |
Single |
29 |
26.1 |
| Married |
81 |
73.0 |
| Divorced |
1 |
0.9 |
| Smoking |
Current smoker |
3 |
2.7 |
| Water pipe smoker |
4 |
3.6 |
| Quit |
5 |
4.5 |
| Never |
99 |
89.2 |
| Family history* |
Yes |
20 |
22.3 |
| Disease characteristics |
pancolitis |
71 |
64.0 |
| Left sided colitis |
40 |
36.0 |
| Extra-intestinal manifestation** |
Yes |
16 |
14.4 |
*At least one of the first/second degree patient’ relatives was affected by inflammatory bowel disease.
**At least one of the following extra-intestinal manifestations was observed: Primary sclerosing cholangitis, erythema nodosum, pyoderma gangrenosum, ankylosing spondylitis, ocular involvement, joint involvement, and pulmonary involvement.
Before colectomy, there were 90 patients (81.0%) on glucocorticosteroids, 91 patients (81.9%) on 5-aminosalsylates, 76 patients (68.4%) on immunomodulators (mostly azathioprine), and 29 patients (26.1%) on anti-TNF alpha compounds.
The most common cause of colectomy was intractable disease in 63 persons (57%), followed by colon cancer or dysplasia in 28 (25%) (Table 2). All the patients were alive when they were discharged from the hospital. Colectomy complications occurred in 44 patients (40%), which were mostly late complications (38, 34%) and led to patients’ re-admission (Table 2).
Table 2.
Reasons for Surgery and Complications Among Colectomy Patients During 10 Years
|
Reasons of surgery, N (%)
|
Intractable disease |
63 (56.8) |
| Fulminant disease |
18 (16.2) |
| Massive colonic hemorrhage |
1 (0.9) |
| Extra-intestinal manifestations |
1 (0.9) |
| Colon dysplasia or cancer |
28 (25.2) |
|
Complications after colectomy, N (%)
|
Early
*
|
Anastomotic lea |
4 (3.6) |
| Sepsis |
1 (0.9) |
| Injury to pelvic nerves |
1 (0.9) |
| Total |
6 (5.4) |
|
Late
*
|
Gastrointestinal bleeding |
3 (2.7) |
| Pouchitis |
13 (11.7) |
| Bowel obstruction |
20 (18.0) |
| Wound infection |
1 (0.9) |
| Deep vein thrombosis |
1 (0.9) |
| Total |
38 (34.2) |
|
Total, N (%)
|
44 (39.6) |
10 years after definite diagnosis.
*Early complications are defined as complications detected in the same admission or within four weeks after colectomy, and late complications are defined as complications diagnosed in subsequent admissions at least four weeks apart. No patient had both complications.
Among 111 records of IBD patients who underwent colectomy, 49 records (44%) were available on phone calls. Seven patients (6.3%) died after colectomy during various periods. The age of six dead patients ranged from 33 to 50 years, and one patient was aged 77 years.
All the 7 dead patients underwent surgery in an urgent setting due to intractable severe exacerbation. Five patients (71.4%) died from advanced colorectal cancer, one (14.3%) from pulmonary thromboembolic problems, and one (14.3%) from bowel obstruction caused by adhesion after surgery. All the dead patients underwent colectomy more than 10 years after definite diagnosis (P value of log rank test <0.001). All deaths occurred within six years after colectomy (Table 3).
Table 3.
Characteristics of Patients who Died after Colectomy
|
Year of Colectomy
|
Age at Colectomy (y)
|
Gender
|
Duration of Disease
*
|
Time Lag
**
|
Cause of Death
|
| 2014–2015 |
45 |
Male |
18 |
36 |
Bowel obstruction due to adhesion after surgery |
| 2016–2017 |
77 |
Female |
62 |
60 |
Colorectal cancer |
| 2016–2017 |
36 |
Male |
18 |
48 |
Colorectal cancer (and primary sclerosing cholangitis) |
| 2016–2017 |
33 |
Female |
14 |
12 |
Pulmonary thromboembolic event |
| 2017–2018 |
46 |
Male |
25 |
36 |
Colorectal cancer |
| 2017–2018 |
40 |
Male |
24 |
12 |
Colorectal cancer |
| 2017–2018 |
50 |
Female |
31 |
12 |
Colorectal cancer |
* Duration from definite diagnosis to death (years).
** Time lag: Duration from colectomy to death (months).
Mean and confidence interval (CI) 95% of survival was 7.7 (6.9–8.6). Three- and five-year survival rates of IBD patients after colectomy were 94% and 84%, respectively (Figure 1).
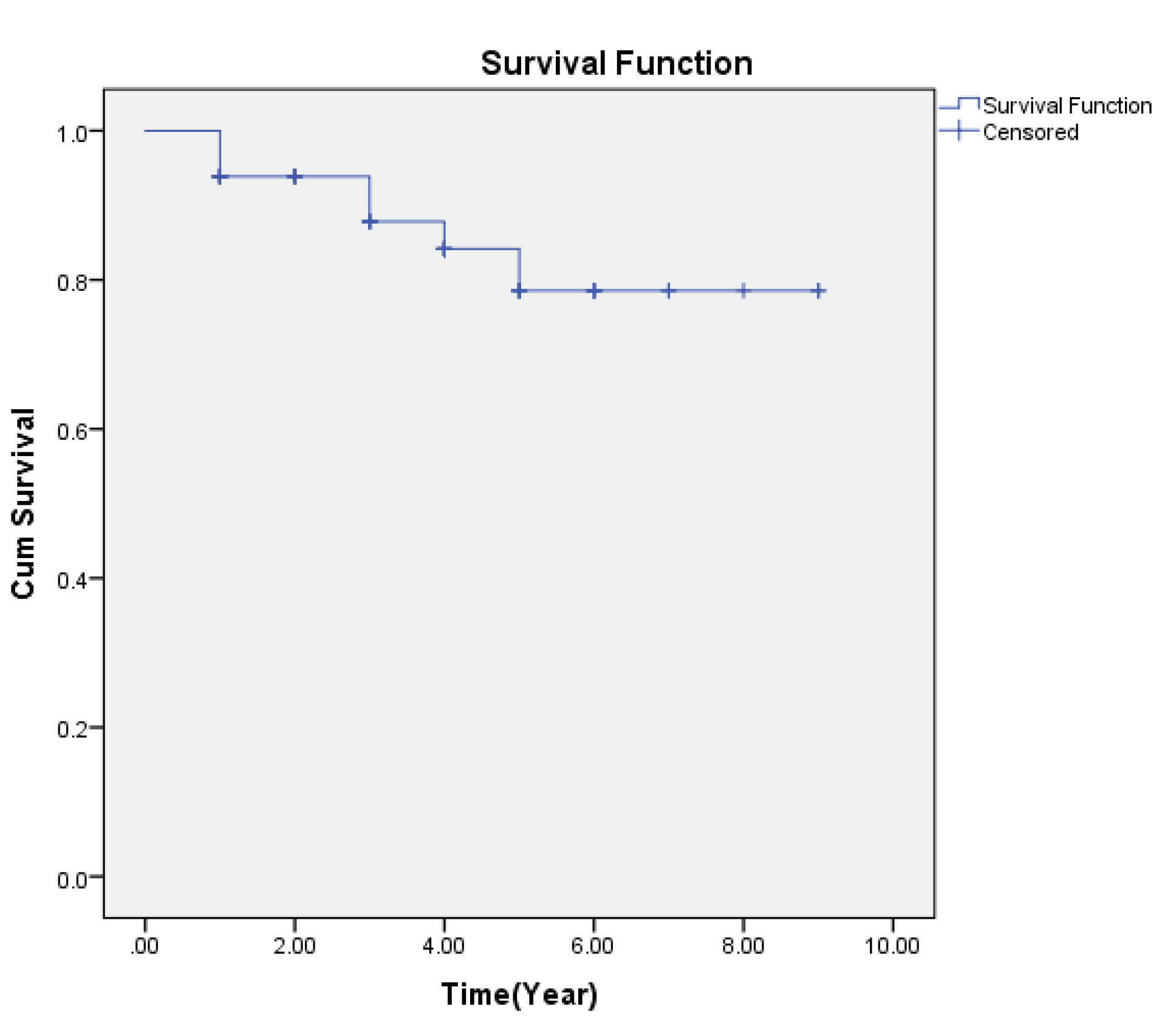
Figure 1.
Survival Rate of Colectomy Patients.
.
Survival Rate of Colectomy Patients.
Table S1 of Supplementary file 1 and Figure 2 show the ratio of patients who received colectomy (C) to total number of admitted UC patients (A) at the same period during 2009 to 2019 as well as the distribution of patients in elective setting of surgery versus urgent/emergent. To standardize the absolute number of colectomy, elective versus urgent/emergent surgery, the frequency was divided by the total UC admissions in the same year.
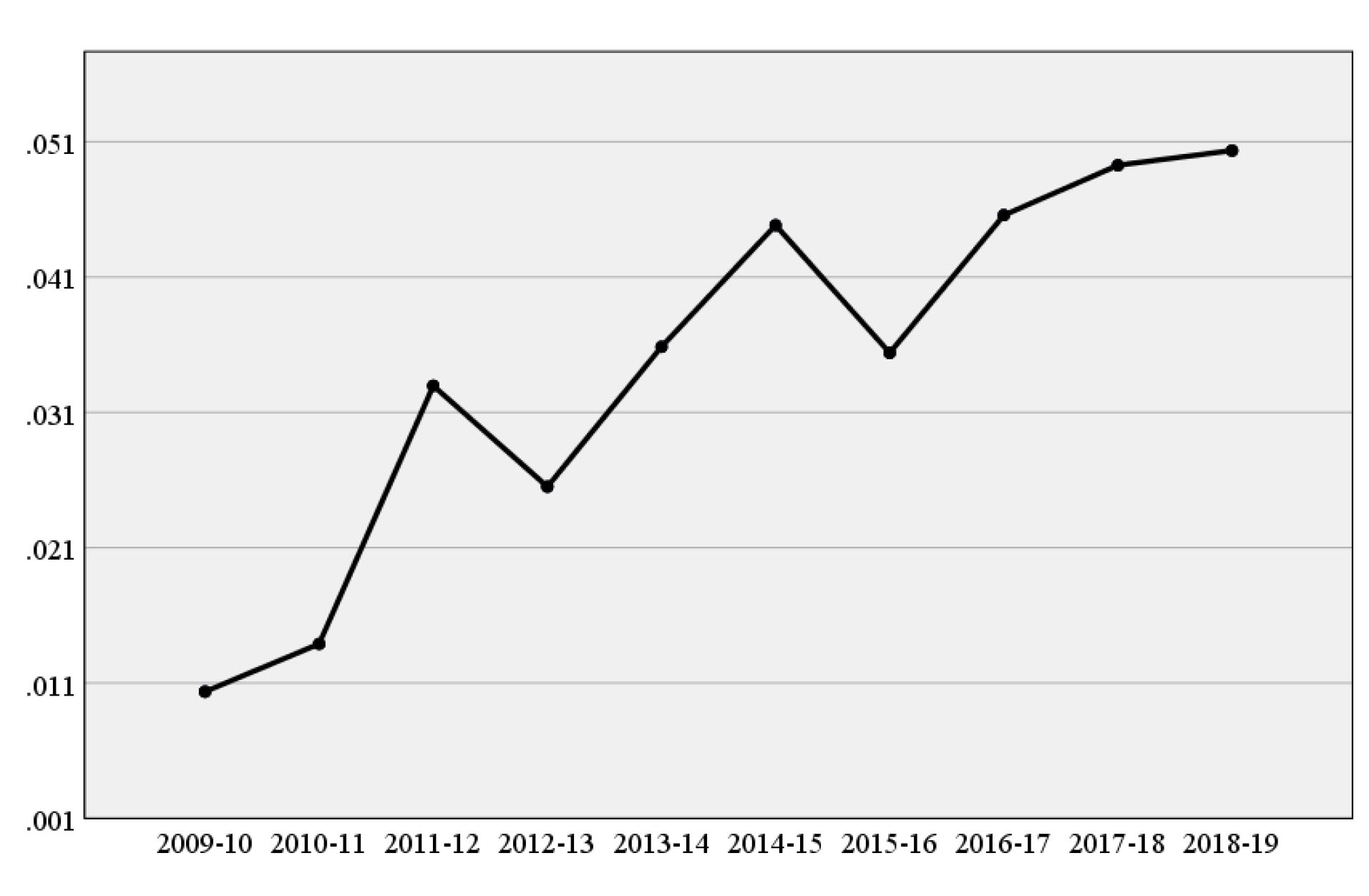
Figure 2.
Trend of the Ratio of Total Frequency of Colectomy to Admissions for Different Years.
.
Trend of the Ratio of Total Frequency of Colectomy to Admissions for Different Years.
The results of Mann-Kendall trend test (Z = 3.39, P < 0.001) showed an upward trend for the ratio of the frequency of colectomies to total UC admissions.
Discussion
This study aimed to show the trend of colectomies for UC patients in Shiraz, southern Iran. The results revealed that despite an increase in UC admissions, the colectomy trend (both elective and urgent/ emergent) increased significantly during a decade.
This occurred despite the avialability of anti-TNF agents (including infliximab and adalimumab) from 2008-2009 in Iran. Both of these compounds are covered by all insurance companies, including the health insurance organization which provides free insurance packages for all individuals not under the insurance coverage of other agencies. Recently, biosimilar Cinnora is produced in Iranain phramacutical companies, and this has made the drug even more afforadbale.
Other studies have shown the decreased rate of colectomy over the last decades.13 Most studies have documented the promising effect of anti-TNF on the reduction of colectomy rate among UC patients,14-16 and even a decrease in the mortality rate of the UC patients.16 In contrast to our finding, a relatively stable trend of colectomy among the UC patients and a falling trend of colectomy incidence for elective surgeries in the biologics era have been reported in Sweden,17 Canada,18,19 and Japan.20
Although part of this difference might be caused by different methodologies and lack of population-based data in our study, the findings could be alarming. IBD, particluarly UC, are rising in Iran; as such, the increase of colectomy rate might be associated with the rising number of these patients.
Another reason could be the inapprpriate use of therapy. Therpautic drug monitoring, which should be incorporated in the management of IBD patinets on biologics, is not widely available in Iran. In this study, adequate dose adjument was probably not performed for these patients. There should be also concerns of compliance to treatment. Irregular dosage of anti-TNF alpha compounds is shown to be associated with lack of response. This highlights the importance of greater empahsis on empowering the patients in chonic care of diseases like IBD.
The collected data indicates that at least half of the patients using anti-TNF alpha treatments would be symptomatic depsite appropriate dosing. This indicates the need for other treatments with other mechanisms, including anti-integrins and small molecules. These alternatives have not been available in Iran until very recently for domestic production of tofactinib. The drug has not been covered yet by major insurance organizations and is not affordable for many IBD patients.
The average lag between diagnosis time and receiving colectomy in our study was 10 years, which is compatible with other reports.11,20 In general, 40% of the patients experienced some kind of post-operative complications. Most complicated patients (34% of all patients) had to be re-admitted to the hospital. These are comparable to the reports from other countries.5-8 Although pouchitis (11.7% of all patients) is included in complications, this could occur due to dysbiosis or altered immunity of patients rather than as a complication of surgery.21
The mortality rate of patients in the present study (6.3%) was higher than the values from other reports which was about half of this figure.5,6,8,10 Three- and five-year survival rates of UC patients undergoing colectomy in this study were 94% and 84%, respectively. This is lower than reports from other series. For example, the data published in South Korea revealed one- and five-year survival rates of 99.7 and 98.7%, respectively.22 More importantly, the majority of the deaths occurred among the younger persons, who underwent urgent surgery.
This may indicative a lag in the decision to perform surgery in those who have unresponsive severe disease.
The cause of death was colorectal cancer in five out of seven patients in whom more than ten years had passed after diagnosis. This highlights the need for more adherence to cancer screening protocols in IBD patients.
To the best of our knowledge, this is the first study to show the increasing trend of colectomy in UC patients in southern Iran in the last decade despite the availability of anti-TNF biologics. The cross-sectional non-population-based nature of this study may limit the results.
In conclusion, despite the use of biologics during the past decade in southern Iran, there was a rising trend in colectomies among UC patients. The frequencies of post-operative complications and mortality were considerable. Most of the dead patients underwent non-elective surgery and were young. This highlights the need for the refinement of UC care in this region.
Supplementary Materials
Supplementary file 1 contains Table S1.
(pdf)
Acknowledgements
The authors would like to thank the authorities of included hospitals for their cooperation. This study was supported by Deputy of research, Shiraz University of Medical Sciences.
Authors’ Contribution
SG: Designed the study, collaborated in data processing, wrote the manuscript, edited and critically reviewed manuscript. MP: Collaborated in collection of data and wrote and critically reviewed the manuscript. MS: Collaborated in analysis and data processing, critically reviewed manuscript. SVH: Collaborated in data processing, edited and critically reviewed manuscript. KBL: Initiated, conceptualized and designed the study, edited and critically reviewed manuscript. All authors approved the final version of the manuscript.
Conflict of Interest Disclosures
Authors have no conflict of interest to declare.
Ethical Statement
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with Helsinki Declaration of 1964 and its later amendments or comparable ethical standards. Ethical approval for this study was obtained from the Ethics Committee of Shiraz University of Medical Sciences (Code of Ethics: IR.SUMS.MED.REC.1397.453).
References
- Podolsky DK. Inflammatory bowel disease (1). N Engl J Med 1991; 325(13):928-37. doi: 10.1056/nejm199109263251306 [Crossref] [ Google Scholar]
- Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J. Harrison’s Principles of Internal Medicine. 19th ed. New York: McGraw-Hill Education; 2015.
- Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol 2008; 103(12):3167-82. doi: 10.1111/j.1572-0241.2008.02158.x [Crossref] [ Google Scholar]
- Taghavi SA, Safarpour AR, Hosseini SV, Noroozi H, Safarpour M, Rahimikazerooni S. Epidemiology of inflammatory bowel diseases (IBD) in Iran: a review of 740 patients in Fars province, Southern Iran. Ann Colorectal Res 2013; 1(1):17-22. doi: 10.17795/acr-11477 [Crossref] [ Google Scholar]
- Kaplan GG, McCarthy EP, Ayanian JZ, Korzenik J, Hodin R, Sands BE. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology 2008; 134(3):680-7. doi: 10.1053/j.gastro.2008.01.004 [Crossref] [ Google Scholar]
- de Silva S, Ma C, Proulx MC, Crespin M, Kaplan BS, Hubbard J. Postoperative complications and mortality following colectomy for ulcerative colitis. Clin Gastroenterol Hepatol 2011; 9(11):972-80. doi: 10.1016/j.cgh.2011.07.016 [Crossref] [ Google Scholar]
- Frolkis A, Kaplan GG, Patel AB, Faris P, Quan H, Jette N. Postoperative complications and emergent readmission in children and adults with inflammatory bowel disease who undergo intestinal resection: a population-based study. Inflamm Bowel Dis 2014; 20(8):1316-23. doi: 10.1097/mib.0000000000000099 [Crossref] [ Google Scholar]
- Ferrante M, Declerck S, De Hertogh G, Van Assche G, Geboes K, Rutgeerts P. Outcome after proctocolectomy with ileal pouch-anal anastomosis for ulcerative colitis. Inflamm Bowel Dis 2008; 14(1):20-8. doi: 10.1002/ibd.20278 [Crossref] [ Google Scholar]
- Dayan B, Turner D. Role of surgery in severe ulcerative colitis in the era of medical rescue therapy. World J Gastroenterol 2012; 18(29):3833-8. doi: 10.3748/wjg.v18.i29.3833 [Crossref] [ Google Scholar]
- Singh S, Al-Darmaki A, Frolkis AD, Seow CH, Leung Y, Novak KL. Postoperative mortality among patients with inflammatory bowel diseases: a systematic review and meta-analysis of population-based studies. Gastroenterology 2015; 149(4):928-37. doi: 10.1053/j.gastro.2015.06.001 [Crossref] [ Google Scholar]
- Parragi L, Fournier N, Zeitz J, Scharl M, Greuter T, Schreiner P. Colectomy rates in ulcerative colitis are low and decreasing: 10-year follow-up data from the Swiss IBD Cohort Study. J Crohns Colitis 2018; 12(7):811-8. doi: 10.1093/ecco-jcc/jjy040 [Crossref] [ Google Scholar]
- Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl 1989; 170:2-6. doi: 10.3109/00365528909091339 [Crossref] [ Google Scholar]
- Frolkis AD, Dykeman J, Negrón ME, Debruyn J, Jette N, Fiest KM. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology 2013; 145(5):996-1006. doi: 10.1053/j.gastro.2013.07.041 [Crossref] [ Google Scholar]
- Sandborn WJ, Rutgeerts P, Feagan BG, Reinisch W, Olson A, Johanns J. Colectomy rate comparison after treatment of ulcerative colitis with placebo or infliximab. Gastroenterology 2009; 137(4):1250-60. doi: 10.1053/j.gastro.2009.06.061 [Crossref] [ Google Scholar]
- Barnes EL, Jiang Y, Kappelman MD, Long MD, Sandler RS, Kinlaw AC. Decreasing colectomy rate for ulcerative colitis in the United States between 2007 and 2016: a time trend analysis. Inflamm Bowel Dis 2020; 26(8):1225-31. doi: 10.1093/ibd/izz247 [Crossref] [ Google Scholar]
- Clemente V, Aratari A, Papi C, Vernia P. Short term colectomy rate and mortality for severe ulcerative colitis in the last 40 years. Has something changed? Dig Liver Dis 2016; 48(4):371-5. doi: 10.1016/j.dld.2015.12.014 [Crossref] [ Google Scholar]
- Eriksson C, Cao Y, Rundquist S, Zhulina Y, Henriksson I, Montgomery S. Changes in medical management and colectomy rates: a population-based cohort study on the epidemiology and natural history of ulcerative colitis in Örebro, Sweden, 1963-2010. Aliment Pharmacol Ther 2017; 46(8):748-57. doi: 10.1111/apt.14268 [Crossref] [ Google Scholar]
- Reich KM, Chang HJ, Rezaie A, Wang H, Goodman KJ, Kaplan GG. The incidence rate of colectomy for medically refractory ulcerative colitis has declined in parallel with increasing anti-TNF use: a time-trend study. Aliment Pharmacol Ther 2014; 40(6):629-38. doi: 10.1111/apt.12873 [Crossref] [ Google Scholar]
- Moore SE, McGrail KM, Peterson S, Raval MJ, Karimuddin AA, Phang PT. Infliximab in ulcerative colitis: the impact of preoperative treatment on rates of colectomy and prescribing practices in the province of British Columbia, Canada. Dis Colon Rectum 2014; 57(1):83-90. doi: 10.1097/dcr.0000000000000003 [Crossref] [ Google Scholar]
- Uchino M, Ikeuchi H, Hata K, Okada S, Ishihara S, Morimoto K. Changes in the rate of and trends in colectomy for ulcerative colitis during the era of biologics and calcineurin inhibitors based on a Japanese nationwide cohort study. Surg Today 2019; 49(12):1066-73. doi: 10.1007/s00595-019-01845-2 [Crossref] [ Google Scholar]
- Shen B. Acute and chronic pouchitis--pathogenesis, diagnosis and treatment. Nat Rev Gastroenterol Hepatol 2012; 9(6):323-33. doi: 10.1038/nrgastro.2012.58 [Crossref] [ Google Scholar]
- Cha JM, Park SH, Rhee KH, Hong SN, Kim YH, Seo SI. Long-term prognosis of ulcerative colitis and its temporal changes between 1986 and 2015 in a population-based cohort in the Songpa-Kangdong district of Seoul, Korea. Gut 2020; 69(8):1432-40. doi: 10.1136/gutjnl-2019-319699 [Crossref] [ Google Scholar]