Arch Iran Med. 24(10):727-732.
doi: 10.34172/aim.2021.107
Original Article
Primary Liver Cancer in Golestan Province, Northeastern Iran: 13-Year Experience of Golestan Population-Based Cancer Registry (GPCR)
Fazel Isapanah Amlashi 1  , Ali Ashkbari 1, Taghi Amiriani 1, Alireza Norouzi 1, Amir Houshang Poorkhani 2, Seyed Mehdi Sedaghat 3, Somayeh Livani 2, Mohammad Ashaari 4, Hamideh Sadeghzadeh 3, Sima Besharat 1, *
, Ali Ashkbari 1, Taghi Amiriani 1, Alireza Norouzi 1, Amir Houshang Poorkhani 2, Seyed Mehdi Sedaghat 3, Somayeh Livani 2, Mohammad Ashaari 4, Hamideh Sadeghzadeh 3, Sima Besharat 1, *  , Shahryar Semnani 1, Gholamreza Roshandel 5
, Shahryar Semnani 1, Gholamreza Roshandel 5
Author information:
1Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran
2Clinical Research Development Unit (CRDU), Golestan University of Medical Sciences, Gorgan, Iran
3Deputy of Public Health, Golestan University of Medical Sciences, Gorgan, Iran
4Deputy of Pathology, Golestan University of Medical Sciences, Gorgan, Iran
5Cancer Research Center, Golestan University of Medical Sciences, Gorgan, Iran
*Corresponding Author: Sima Besharat, MD, PhD; Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran. Address: Research Center complex, 3rd floor, Salim heart complex, Sayyad-e-Shirazi hospital, Sayyad-e-Shirazi Boulevard, Gorgan city, Golestan Province, Postal code: 49178-67439, Iran. Tel: +98-911-375-8264; Fax: +98-17-32251910; Email:
s_besharat_gp@yahoo.com
Abstract
Background:
Liver cancer (LC) is among the most common and fatal cancers worldwide. A four-fold increasing trend is reported for LC age-standardized mortality rate (ASMR) in Iran within 1990–2015. In the present study, we aimed to report the incidence rate of LC during the 13-year establishment of the Golestan population-based cancer registry (GPCR).
Methods:
Age-standardized incidence rate (ASIR) per 100000 person-years was calculated using CanReg5 software. The Joint point regression analysis was used to assess the temporal trends in incidence rate of LC.
Results:
During the study period, GPCR registered 575 of LC cases, of which 373 (64.9%) were men and 297 (51.6%) lived in rural areas. The mean (SD) age of LC in men and women were 60.3 (17.2) and 58.0 (17.1), respectively. The ASIR of LC was significantly higher in men than women (4.7 vs. 2.6; P value<0.01) and a minimal increasing trend in LC incidence was observed in both sexes. The incidence rate of LC was significantly higher in rural areas compared to the urbans (3.91 vs. 3.40; P value=0.04). In the last 13 years, rural population had a significant increasing trend in ASIR of LC (average annual percent change [AAPC]=7.85, P value=0.005).
Conclusion:
LC was more prevalent in men among both urban and rural populations. The results showed a significant increasing trend in rural areas that requires Golestan health care system to take action in controlling the burden of LC in rural areas.
Keywords: Age-standardized incidence rates, Golestan population-based based cancer registry, Hepatocellular carcinoma, Iran, Liver cancer
Copyright and License Information
© 2021 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Isapanah Amlashi F, Ashkbari A, Amiriani T, Norouzi A, Poorkhani AH, Sedaghat SM, et al. Primary liver cancer in golestan province, northeastern iran: 13-year experience of golestan population-based cancer registry (gpcr). Arch Iran Med. 2021;24(10):727-732. doi: 10.34172/aim.2021.107
Introduction
Liver cancer (LC), in 2018, ranked number 6 in the list of most common cancers with about 81 400 new cases and ranked number 4 in leading causes of cancer-related deaths around the world with 78 200 deaths.1,2 In 2017, the age-standardized incidence rate (ASIR; per 100 000 person-year) and age-standardized mortality rate (ASMR; per 100 000 people) of LC were reported to be 10.1 and 9.5, respectively.3 GLOBOCAN 2018 reported that the highest incidence and mortality rates of LC for both sexes pertain to Eastern Asia (ASIR: men = 26.8, women = 8.7), Southeastern Asia (ASIR: men = 21, women = 6.6), and Northern Africa (ASIR: men = 20.8, women = 7.8).1,3-5 After Asia and Africa, the highest rates in the world in 2018 occurred in Southern Europe (ASIR: men = 10.9, women = 3.4) followed by North America (ASIR: men = 9.4, women = 3.4), and the lowest ASIR (men = 5.8, women = 3.5) are observed in South America.1 Eighty-five percent of new cases were reported in developing countries due to lack of appropriate diagnostic and treatment facilities.6,7 But new studies indicate that the LC incidence has decreased about 20% in areas with high incidence such as China and Japan, in contrast to low incidence areas.4,8 Also, most of the studies showed an increase in the incidence of LC by 37.6% from 2006 to 2016 in the world which may be explained to some extent by the population growth and aging.9-11
The highest incidences of LC are reported in Asia. The high incidence of LC in Asia might be due to the fact that 75% of patients with chronic hepatitis B were in it until 2017.6,12 In this continent, Mongolia has the world’s highest ASIR of LC (78.1 per 100 000) and Nepal has the lowest ASIR of LC (0.9) worldwide.8,13
Iran is located in a region with low risk of LC for both sexes.11,14 According to the results of a meta-analysis in Iran from 1996 to 2016, the ASIR of LC was 1.66 for males and 1.25 for females.14 Studies in 2012, based on all registered Iranian cancer cases, showed 1567 patients with LC.13 The articles pointed to scattered results but reported that some provinces including Ardebil, Semnan, and Khuzestan had the highest incidence of LC in Iran.11 As previous studies indicated, the incidence of LC in Iran, as well as changes in global epidemiology, is increasing.11,15 The exact increasing rate for Iran is not specified, but in one study from 1990 to 2006, this rate was about 0.2.15 According to GLOCOBAN 2018 in Golestan, 157 (94 male, 63 female) new cases of LC were reported, indicating ASIR of 3.9 in males and 2.5 in females.16
Primary LC has different types, but the most common cases include hepatocellular carcinoma or HCC (comprising 75%‒85% of cases) and cholangiocarcinoma or bile duct cancer (comprising 10%‒15% of cases).1,8 Important risk factors of LC include sex, chronic viral hepatitis (hepatitis B virus [HBV] and hepatitis C virus [HCV]), cirrhosis, alcohol consumption, diabetes, and smoking.8,17 LC incidence and mortality are 2‒3 times higher in men than women around the world.1,18 Genetic and behavioral factors might influence men more than women.14 New research suggests that chronic infections with HBV and HCV are responsible for almost three-quarters (73.4%) of HCC.6,19 HBV vaccination programs in some countries such as Japan and Taiwan caused considerable changes in the epidemiology of liver disease.6,19
Considering the recent increase in LC incidence in Iran and the high prevalence of gastrointestinal cancers in Golestan,16 the present study was designed to investigate 13-year incidence rate and its temporal and geographical distribution in Golestan, Iran between 2004 and 2016.
Materials and Methods
The Golestan province is located in northern Iran, with a total population of 1 868 819 (938 327 (50.21%) men; 930 492 (49.79%) women) in 2016.20 Golestan population-based cancer registry (GPCR) registers primary incident cases of cancers noting all standards of the International Agency for Research on Cancer and International Association of Cancer Registries.21 All LC cases registered by GPCR during 2004‒2016 were enrolled in this study.
The methodology of cancer registry in GPCR was completely described in GPCR establishment before.21 In brief; the GPCR collects data using passive and active methods from all public and private diagnostic and therapeutic centers including hospitals, pathology/laboratory centers, imaging centers and selected specialists’ offices. Data about cancer-related deaths were collected from death registry at the Health Department of Golestan University of Medical Sciences (GOUMS). Comparison of 10% of collected data to original documents is used in order to verify the accuracy of the data gathering process.21 The third edition of the international classification of disease for oncology (ICD-O-3) is used for coding tumor features.21,22 CanReg5 software is used for calculating ASIR of LC.21,23 The ASIRs were calculated using direct standardization method24 and the 18-group world population25 was considered as the standard population.
In this study, joinpoint regression analysis was considered for time trend analysis using the joinpoint regression program version 4.6.0.0.26 Average annual percent change (AAPC) and 95% confidence interval (CI) were calculated. Heteroscedasticity was handled by using weighted least squares. Autocorrelation was taken into account by the method described by Kim et al.27
Results
During the study period, GPCR registered 575 of LC cases, of which 373 (64.9%) were males and 202 (35.1%) were females. The mean (SD) age of LC patients was 60.3 (17.2) and 58.0 (17.1) in males and females, respectively.
Overall, the ASIR and the crude rate of LC in the Golestan population were 2.55 and 3.64 per 100 000 person-years, respectively. Table 1 shows the numbers, crude rate, ASIRs, and 95% CI of ASIRs of LC in Golestan by sex and residence during 2004–2016.
Table 1.
Numbers, Crude Rate, Age Standardized Incidence Rates (ASIRs) and 95% Confidence Intervals (CI) of ASIRs of Primary Liver Cancers in Golestan Province, Iran by Sex, Residence Area and Year (2004–2016)
|
|
Male
|
Female
|
|
Number
|
Crude Rate
|
ASIR
|
95% CI of ASIR
|
Number
|
Crude Rate
|
ASIR
|
95% CI of ASIR
|
| Residence |
Total |
373 |
3.3 |
4.7 |
4.2–5.2 |
202 |
1.8 |
2.6 |
2.2–2.9 |
| Urban |
184 |
3.2 |
4.5 |
3.8–5.2 |
94 |
1.6 |
2.2 |
1.8–2.7 |
| Rural |
189 |
3.4 |
5.0 |
4.2–5.7 |
108 |
1.9 |
2.9 |
2.3–3.5 |
Figure 1 shows age-specific incidence rates (per 100 000 person-years) of LC in the province by gender. The age-specific incidence rates of LC in Golestan by residence are presented in Figure 2. Table 2 shows the results of joinpoint analysis for time trends in the incidence of LC in the Golestan province, Iran (2004‒2016), by sex and residence area. Figures 3 and 4 show the temporal variations in ASIR of LC in the Golestan province, based on sex and residence, respectively.
Table 2.
Time Trends in Incidence of Primary Liver Cancers in Golestan Province, Iran (2004‒2016), by Gender and Residence Area
|
|
|
Time Period
|
AAPC
|
95% CI of AAPC
|
P
Value
|
| Gender |
Male |
2004–2016 |
2.40 |
-2.21 to 7.23 |
0.281 |
| |
Female |
2004–2016 |
1.69 |
-6.93 to 11.10 |
0.690 |
| Residence |
Urban |
2004–2016 |
1.75 |
-2.81 to 6.53 |
0.420 |
|
|
Rural |
2004–2016 |
7.85 |
2.88 to 13.07 |
0.005 |
AAPC, Average Annual Percent Change of Incidence Rates; CI, Confidence Interval.
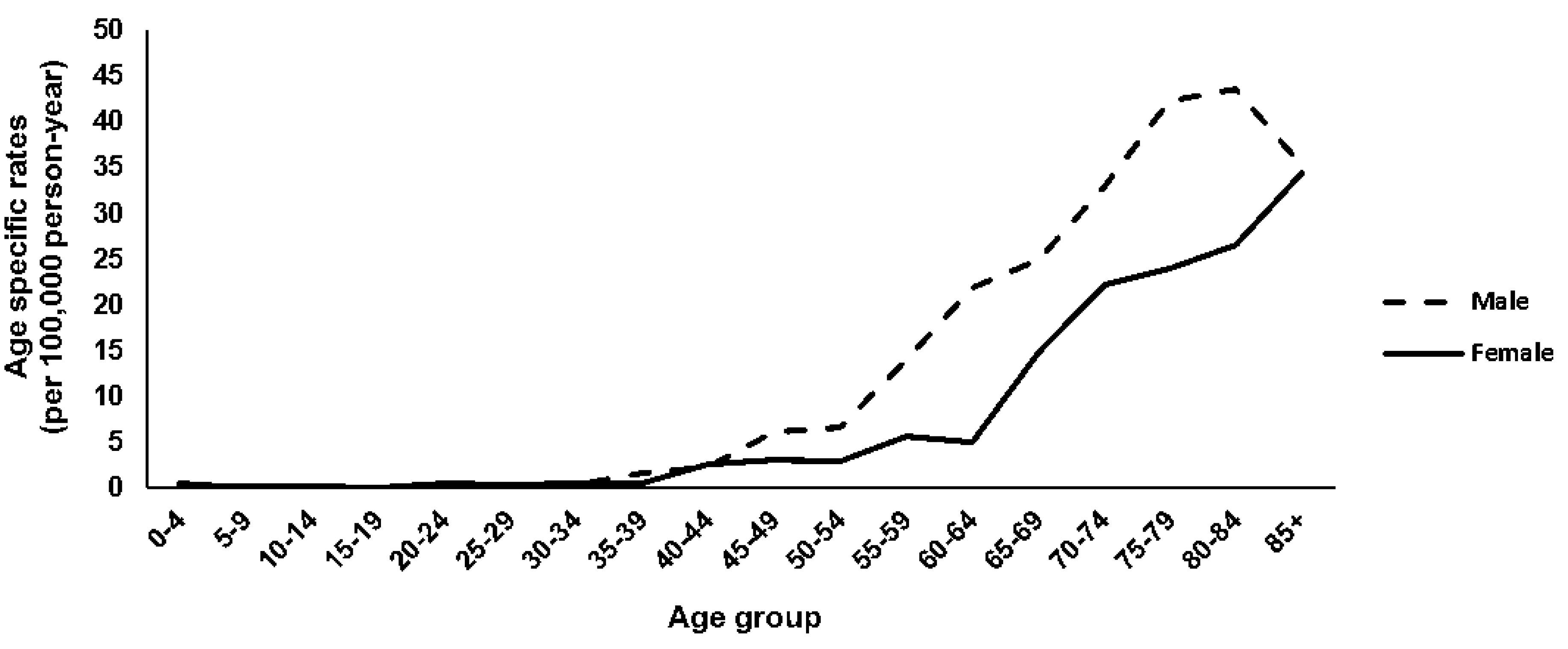
Figure 1.
Age-Specific Incidence Rates (Per 100 000 Person-Years) of Primary Liver Cancers in Golestan Province, Iran by Gender (2004–2016).
.
Age-Specific Incidence Rates (Per 100 000 Person-Years) of Primary Liver Cancers in Golestan Province, Iran by Gender (2004–2016).
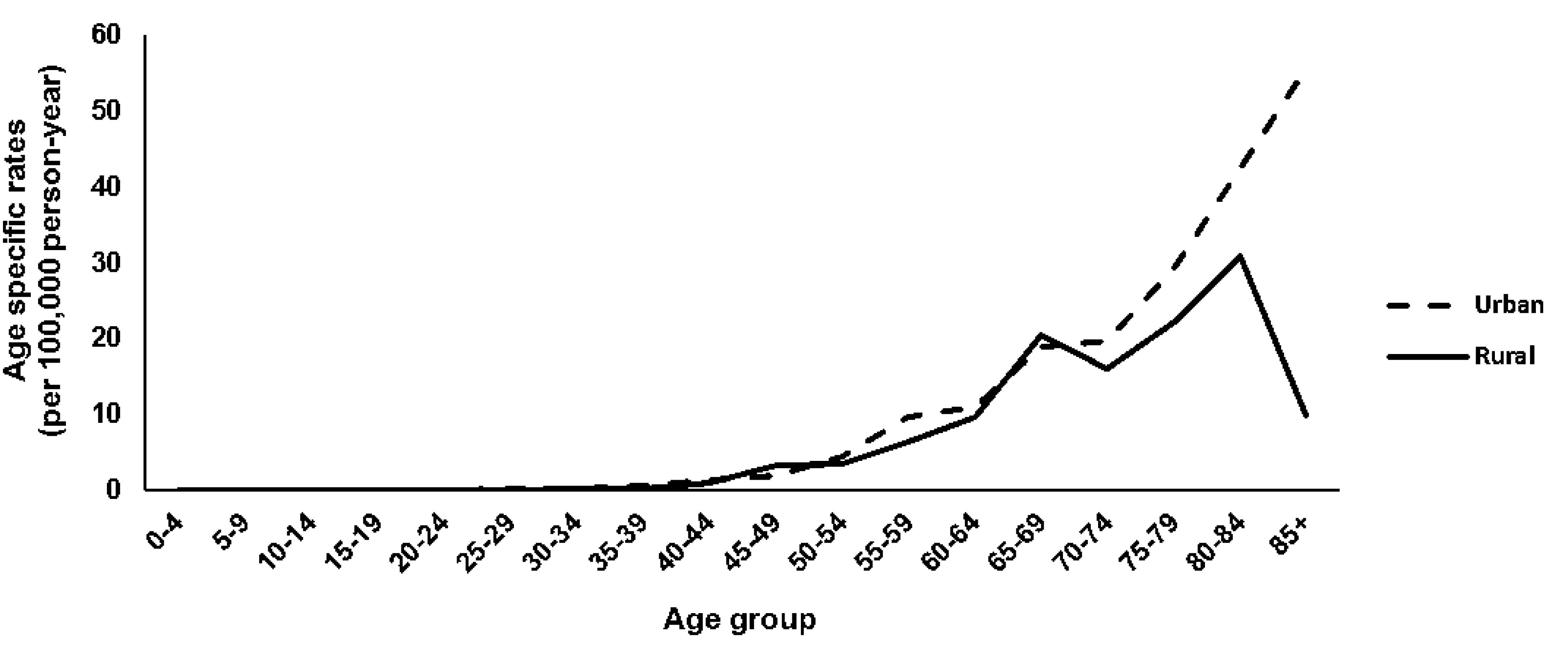
Figure 2.
Age-Specific Incidence Rates (Per 100 000 Person-Years) of Primary Liver Cancers in Golestan Province, Iran by Residence Area (2004–2016).
.
Age-Specific Incidence Rates (Per 100 000 Person-Years) of Primary Liver Cancers in Golestan Province, Iran by Residence Area (2004–2016).
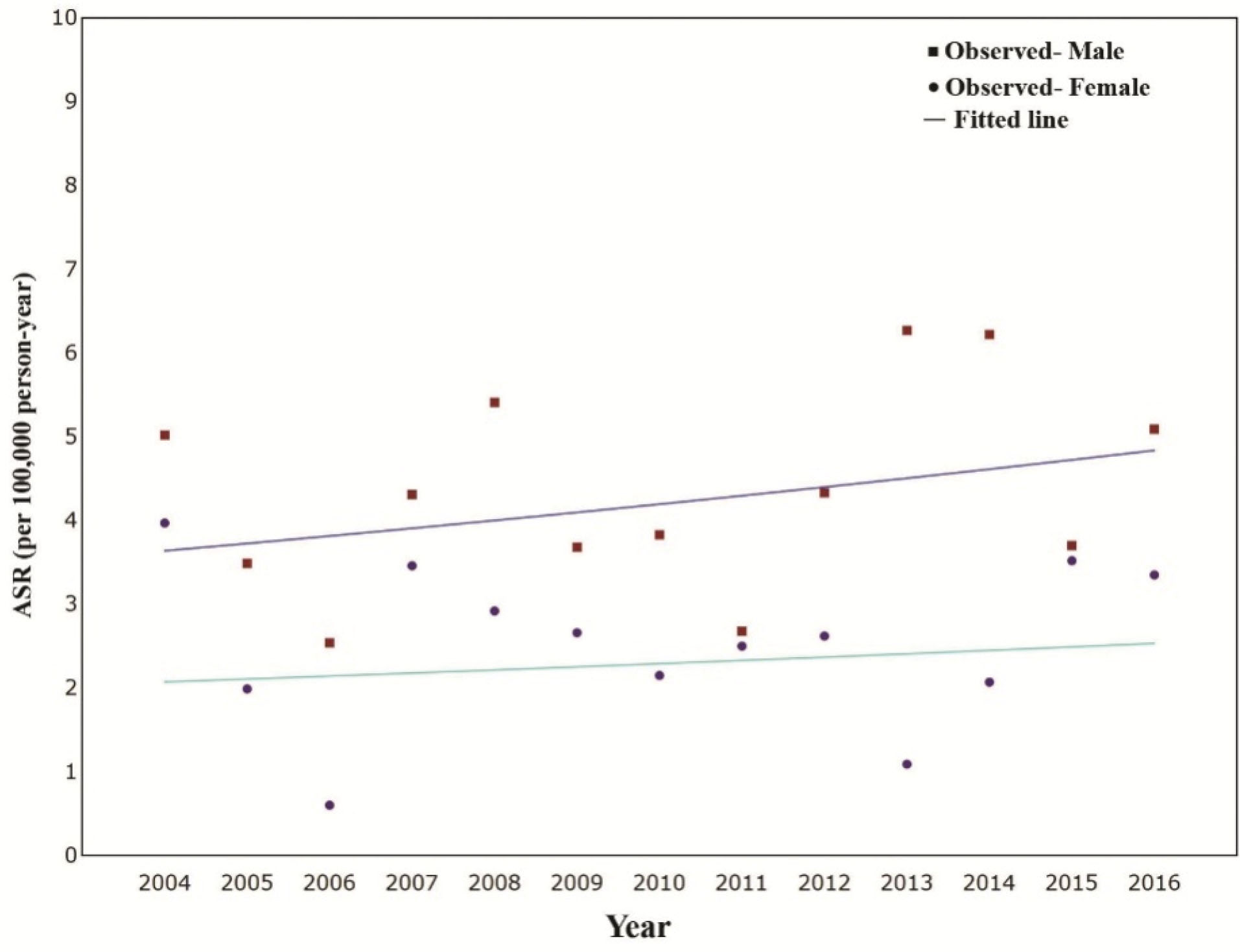
Figure 3.
Temporal Variations in Age-Standardized Incidence Rates (ASIR), Per 100 000 Person-Years, of Primary Liver Cancers in Golestan Province, Iran, by Gender (2004–2016).
.
Temporal Variations in Age-Standardized Incidence Rates (ASIR), Per 100 000 Person-Years, of Primary Liver Cancers in Golestan Province, Iran, by Gender (2004–2016).
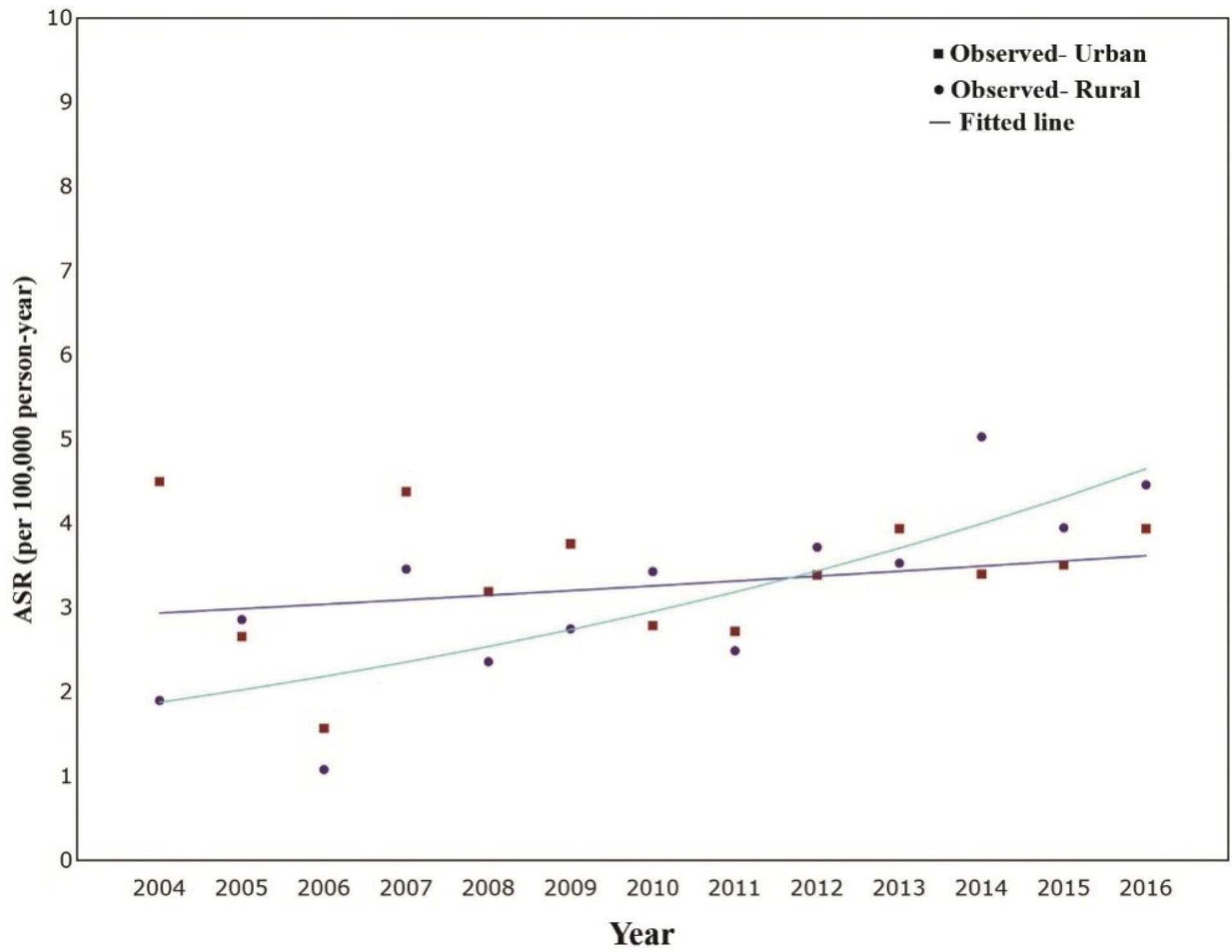
Figure 4.
Temporal Variations in Age-Standardized Incidence Rates (ASIR), Per 100 000 Person-Years, of Primary Liver Cancers in Golestan Province, Iran, by Residence (2004–2016).
.
Temporal Variations in Age-Standardized Incidence Rates (ASIR), Per 100 000 Person-Years, of Primary Liver Cancers in Golestan Province, Iran, by Residence (2004–2016).
As presented in Table 2 and Figure 3, we found slight increasing trends in the incidence of LC in males (AAPC = 2.40; 95% CI: -2.21–7.23; P value = 0.28) and females (AAPC = 1.69; 95% CI: -6.93–11.10; P value = 0.69), although the trends were not statistically significant. The ASIR of LC was significantly higher in males (4.7; 95% CI: 4.2–5.2) than females (2.6; 95% CI: 2.2–2.9) (Table 1) (P value < 0.01) (mean difference: 2.1; 95% CI: 1.3–2.9).
As presented in Table 2 and Figure 4, our results showed a significant increasing trend in ASIR of LC in rural areas (AAPC = 7.85; 95% CI: 2.88 – 13.07; P value = 0.005), but no significant trends were found in the urban population (AAPC = 1.75; 95% CI: -2.81–6.53; P value = 0.42). The ASIR of LC was higher in the rural population (3.9; 95% CI: 3.4–4.4) than urban residents (3.4; 95% CI: 3.0‒3.8) (P value = 0.57) (mean difference: 0.5; 95% CI: -0.2–1.2).
Discussion
The ASIR of LC
The present study was designed on the basis of GPCR to investigate the 13-year incidence rate of LC and its temporal and geographical distribution in Golestan, Iran between 2004 and 2016. During the period of the study, 575 cases (64.9% male) of LC were registered. The ASIR of LC and the crude rate were 3.64 and 2.55, respectively.
From 1990 to 2015, the incident case of LC increased by 75%; during this period of time, the ASIR in the United States, Canada, Australia and most parts of Europe increased over 100% while high incidence areas such as China and countries in Western and Eastern sub-Saharan Africa showed a decrease of over 20% with Iran experiencing a minimal growth in incidence.28 The top two high risk areas of LC in the world are located in Eastern and South-Eastern Asia but the lowest incidence was reported from Western Asia.1 The ASIR of LC in high Human Development Index21 areas and low HDI areas among men and women were 16.5, 8.5, 5.5, and 3.5, respectively.1 East Asian countries including China and Korea have higher HDI than West Asian countries, including the Middle East.1 Iran as a Middle Eastern country has lower ASIR of LC in both sexes compared to other countries of this group but a slight trend was reported in the incidence of LC between 2004 to 2016 in the Golestan province. This increase could be due to population growth alongside others risk factors.
Rural vs. Urban Regions
According to the results of our population-based study, significant temporal changes were detected in the incidence rate of LC in both urban and rural parts. From 2004 to 2016, the ASIR of urban areas in Golestan only had a minimal rising trend while the ASIR of rural areas increased considerably, which could be the results of lifestyle changes during this time. Epidemic obesity and some traditional habits like “bloodletting” on the mastoid behind the ear (called “posht gosh zadan” in Persian) is believed to treat jaundice in newborns in some areas of the Golestan province (“Aliabad”, “Khanbibin”, and “Azadshahr”) and could be considered as a transmission way of HBV and HCV. During the early years, rural areas had lower ASIR of LC but the accelerating pace of ASIR increasing trend led to higher ASIR in rural areas than urban areas after 2012. The results of studies from China reported the rural LC incidence rate to be higher than urban parts,29,30 although a prominent decreasing trend was seen in some regions due to the more extensive coverage of HBV vaccination in recent years.30 On the other hand, similar incidence of LC was reported in urban and rural areas in some studies.31
Females vs. Males
In this study, increasing trends were seen in both sexes with a significantly higher incidence rate in males compared to females. According to GLOCOBAN 2018, 596,574 of LC cases around the world were male and 244,506 were female. The global ASIR of LC in females and males were 4.9 and 13.9, respectively. The highest ASIR of LC in males was observed in Mongolia (males: 26.8) and females in Melansia (females: 8.9) worldwide. In most parts of the world, both incidence and mortality rates were around 2 to 3 times higher in men. In Western Asia, the ASIR of LC in males and females were 5.4 and 2.8, respectively.1 Although the incidence of LC in the Golestan population in both sexes is lower than the global rate, it is more common in men. Tobacco use, alcohol consumption, and IV drug abuse are parts of lifestyle factors which are more common among men18 while cultural traditions in the Golestan population limit women from experiencing them.
Age
Our results show the increased risk of LC with age but a declining trend were observed in the 80-84 and 85+ age groups in men. Rural parts also show the same declining trend of LC incidence among ages 80 and over. The results of a recent study in China in 1990‒2017 indicated the increased risk of LC incidence with age but its ascending incidence stopped in the 80‒84 age group in men.32 The elderly population are more susceptible to the disease, injuries, and risk factors. In addition, the cumulative exposure of the elderly to risk factors is rising too.32 Considering the fact the population aged 65 and over is growing all over the world, the number of people at high risk of LC will increase in the future.33
Exposure to the LC Risk Factors
The most important additional risk factors of LC (mainly HCC) are HCV, HBV,34 alcohol, tobacco, obesity and aflatoxin.35 The high incidence of infection with HBV in Golestan could be the main cause of high HCC incidence in this province.36 Studies suggest that vaccination effect may have started in 2006 because of declined HBV infections in Iran after this time.37,38 Considering the very low prevalence of HCV-infected cases in this area,39 it seems that HBV could be considered as the main cause of almost every virus-related HCC cases.
The rising incidence of non-alcoholic fatty liver disease and the obesity epidemic,40,41 and dietary exposure to aflatoxin42 are among other important factors of the accelerating pace of LC incidence in the future in Golestan.
Medical Technologies
Medical technologies, as one of the main bases of diagnosis, play an important role in the increasing number of diagnoses. Over the years, medical technology for diagnosis of LC in the Golestan province has made a significant progress. Besides, during this study, the number of gastroenterologists and hepatologists increased significantly in Golestan. This progress in both medical technology and experts could be relevant to the increase in the incidence of LC in Golestan during this period of time.
Limitation
The small sample size, especially in some subgroups, was the most important limitation of this study. This limitation, represented as wide confidence intervals and consequently, lack of precision in some subgroups should be considered in interpretation of our findings.
In conclusion,the results of the present study show that the LC incidence is higher in rural areas of Golestan. The higher rate of LC was observed in men in both urban and rural areas. Considering the significant increasing trend of LC in rural areas, further investigations are needed to clarify the epidemiologic aspects of it. It is suggested that Golestan health care system plan for handling this growing burden of LC in rural areas.
Acknowledgements
The authors appreciate the GPCR staff, medical professions and personnel of healthcare centers throughout the Golestan province, and also research deputy of Golestan University of Medical sciences (GOUMS) for financial support.
Authors’ Contribution
FIA and AA contributed in drafting the article, critical revision of the article and final approval of the version to be published. TA, AN, AHP and SHS contributed in conception and design of the work, data collection and data analysis and interpretation, and the final approval of the version to be published. SMS, SL, MA and HS participated in the design and interpretation of the data; and performed the project and analysis. And also participated in the first drafting of paper. SB and GHR conceived this research and designed the project, wrote the paper and participated in the revisions of it. All authors read and approved the final manuscript and take responsibility for the content of the work submitted for review.
Conflict of Interest Disclosures
The authors reported that they have no conflict of interest.
Ethical Statement
This project has been approved in the local ethical committee of Golestan University of Medical Sciences.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68(6):394-424. doi: 10.3322/caac.21492 [Crossref] [ Google Scholar]
- Ding C, Fu X, Zhou Y, Liu X, Wu J, Huang C. Disease burden of liver cancer in China from 1997 to 2016: an observational study based on the Global Burden of Diseases. BMJ Open 2019; 9(4):e025613. doi: 10.1136/bmjopen-2018-025613 [Crossref] [ Google Scholar]
- Mohammadian M, Mahdavifar N, Mohammadian-Hafshejani A, Salehiniya H. Liver cancer in the world: epidemiology, incidence, mortality and risk factors. World Cancer Res J 2018; 5(2):e1082. doi: 10.32113/wcrj_20186_1082 [Crossref] [ Google Scholar]
- Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends--an update. Cancer Epidemiol Biomarkers Prev 2016; 25(1):16-27. doi: 10.1158/1055-9965.epi-15-0578 [Crossref] [ Google Scholar]
- Mahdavi S, Amoori N, Salehiniya H, Enayatrad M. Epidemiology and trends in mortality from liver cancer in Iran. Int J Epidemiol Res 2015; 2(4):239-40. [ Google Scholar]
- Wong MCS, Huang JLW, George J, Huang J, Leung C, Eslam M. The changing epidemiology of liver diseases in the Asia-Pacific region. Nat Rev Gastroenterol Hepatol 2019; 16(1):57-73. doi: 10.1038/s41575-018-0055-0 [Crossref] [ Google Scholar]
- Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol 2017; 3(4):524-48. doi: 10.1001/jamaoncol.2016.5688 [Crossref] [ Google Scholar]
- Lange N, Dufour JF. Changing epidemiology of HCC: how to screen and identify patients at risk?. Dig Dis Sci 2019; 64(4):903-9. doi: 10.1007/s10620-019-05515-8 [Crossref] [ Google Scholar]
- Signore G, Nicod-Lalonde M, Prior JO, Bertagna F, Muoio B, Giovanella L. Detection rate of radiolabelled choline PET or PET/CT in hepatocellular carcinoma: an updated systematic review and meta-analysis. Clin Transl Imaging 2019; 7(4):237-53. doi: 10.1007/s40336-019-00332-5 [Crossref] [ Google Scholar]
- Fitzmaurice C, Akinyemiju TF, Al Lami FH, Alam T, Alizadeh-Navaei R, Allen C. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: a systematic analysis for the global burden of disease study. JAMA Oncol 2018; 4(11):1553-68. doi: 10.1001/jamaoncol.2018.2706 [Crossref] [ Google Scholar]
- Farhood B, Raei B, Malekzadeh R, Shirvani M, Najafi M, Mortezazadeh T. A review of incidence and mortality of colorectal, lung, liver, thyroid, and bladder cancers in Iran and compared to other countries. Contemp Oncol (Pozn) 2019; 23(1):7-15. doi: 10.5114/wo.2019.84112 [Crossref] [ Google Scholar]
- Besharat S, Poustchi H, Mohamadkhani A, Katoonizadeh A, Moradi A, Roshandel G. Association of mutations in the basal core promoter and pre-core regions of the hepatitis B viral genome and longitudinal changes in HBV level in HBeAg negative individuals: results from a cohort study in northern Iran. Hepat Mon 2015; 15(2):e23875. doi: 10.5812/hepatmon.23875 [Crossref] [ Google Scholar]
- Ghamari ZT, Tadayon F, Mazdak H. Prevalence of liver cancer in Isfahan province, Iran. Indones J Cancer 2018; 12(2):56-9. doi: 10.33371/ijoc.v12i2.578 [Crossref] [ Google Scholar]
- Hassanipour S, Mohammadzadeh M, Mansour-Ghanaei F, Fathalipour M, Joukar F, Salehiniya H. The incidence of hepatocellular carcinoma in Iran from 1996 to 2016: a systematic review and meta-analysis. J Gastrointest Cancer 2019; 50(2):193-200. doi: 10.1007/s12029-019-00207-y [Crossref] [ Google Scholar]
- Mirzaei M, Ghoncheh M, Pournamdar Z, Soheilipour F, Salehiniya H. Incidence and trend of liver cancer in Iran. J Coll Physicians Surg Pak 2016; 26(4):306-9. [ Google Scholar]
- Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R, et al. Cancer Incidence in Five Continents. IARC Scientific Publication; 2017.
- Su CH, Lin Y, Cai L. Genetic factors, viral infection, other factors and liver cancer: an update on current progress. Asian Pac J Cancer Prev 2013; 14(9):4953-60. doi: 10.7314/apjcp.2013.14.9.4953 [Crossref] [ Google Scholar]
- Cocker F, Chien Yee K, Palmer AJ, de Graaff B. Increasing incidence and mortality related to liver cancer in Australia: time to turn the tide. Aust N Z J Public Health 2019; 43(3):267-73. doi: 10.1111/1753-6405.12889 [Crossref] [ Google Scholar]
- Petrick JL, McGlynn KA. The changing epidemiology of primary liver cancer. Curr Epidemiol Rep 2019; 6(2):104-11. doi: 10.1007/s40471-019-00188-3 [Crossref] [ Google Scholar]
- Population of Golestan in 2016. Available from: https://www.amar.org.ir/news/ID/2504.
- Roshandel G, Semnani S, Fazel A, Honarvar M, Taziki M, Sedaghat S. Building cancer registries in a lower resource setting: The 10-year experience of Golestan, northern Iran. Cancer Epidemiol 2018; 52:128-33. doi: 10.1016/j.canep.2017.12.014 [Crossref] [ Google Scholar]
- Fritz A. International Classification of Diseases for Oncology: ICD-O. Geneva: World Health Organization; 2000.
- Ervik MJ, Cooke AP, Ferlay J, Rahimi A, Antomi S, Dhivar D, et al. CanReg5: Computer Software for Cancer Registries. Lyon: International Agency for Research on Cancer (IARC); 2008.
- Jensen OM. Cancer Registration: Principles and Methods. Lyon: International Agency for Research on Cancer (IARC); 1991.
- Segi M, Fujisaku S. Cancer Mortality for Selected Sites in 24 Countries (1950-1957): Department of Public Health. Tohoku University School of Medicine; 1960.
- Statistical Research and Applications Branch. Joinpoint Regression Program. Version 4.6.0.0 ed. 2018.
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000; 19(3):335-51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z [Crossref] [ Google Scholar]
- Akinyemiju T, Abera S, Ahmed M, Alam N, Alemayohu MA, Allen C. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the global burden of disease study 2015. JAMA Oncol 2017; 3(12):1683-91. doi: 10.1001/jamaoncol.2017.3055 [Crossref] [ Google Scholar]
- Chen WQ, Zheng RS, Zhang SW. Liver cancer incidence and mortality in China, 2009. Chin J Cancer 2013; 32(4):162-9. doi: 10.5732/cjc.013.10027 [Crossref] [ Google Scholar]
- Zheng R, Qu C, Zhang S, Zeng H, Sun K, Gu X. Liver cancer incidence and mortality in China: temporal trends and projections to 2030. Chin J Cancer Res 2018; 30(6):571-9. doi: 10.21147/j.issn.1000-9604.2018.06.01 [Crossref] [ Google Scholar]
- Cao XQ, Cao RF, Liu SZ, Chen Q, Quan PL, Luo SX. Incidence and mortality of liver cancer in Henan province in 2015. Chronic Dis Transl Med 2019; 5(3):197-202. doi: 10.1016/j.cdtm.2019.08.005 [Crossref] [ Google Scholar]
- Wang F, Mubarik S, Zhang Y, Wang L, Wang Y, Yu C. Long-term trends of liver cancer incidence and mortality in China 1990-2017: a joinpoint and age-period-cohort analysis. Int J Environ Res Public Health 2019; 16(16). doi: 10.3390/ijerph16162878 [Crossref]
- Noroozian M. The elderly population in Iran: an ever growing concern in the health system. Iran J Psychiatry Behav Sci 2012; 6(2):1-6. [ Google Scholar]
- Moossavi S, Besharat S, Sharafkhah M, Ghanbari R, Sharifi A, Rezanejad P. Inverse association of plasma level of glutathione peroxidase with liver fibrosis in chronic hepatitis B: potential role of iron. Middle East J Dig Dis 2016; 8(2):122-30. doi: 10.15171/mejdd.2016.17 [Crossref] [ Google Scholar]
- Sia D, Villanueva A, Friedman SL, Llovet JM. Liver cancer cell of origin, molecular class, and effects on patient prognosis. Gastroenterology 2017; 152(4):745-61. doi: 10.1053/j.gastro.2016.11.048 [Crossref] [ Google Scholar]
- Poustchi H, Katoonizadeh A, Ostovaneh MR, Moossavi S, Sharafkhah M, Esmaili S. Cohort profile: Golestan hepatitis B cohort study- a prospective long term study in northern Iran. Middle East J Dig Dis 2014; 6(4):186-94. [ Google Scholar]
- Mohammadi Z, Keshtkar A, Eghtesad S, Jeddian A, Pourfatholah AA, Maghsudlu M. Epidemiological profile of hepatitis B virus infection in Iran in the past 25 years; a systematic review and meta-analysis of general population studies. Middle East J Dig Dis 2016; 8(1):5-18. doi: 10.15171/mejdd.2016.01 [Crossref] [ Google Scholar]
- Moradi A, Khodabakhshi B, Roshandel G, Kalavi K, Besharat S, Semnani S. Response to the hepatitis B virus vaccine in Iranian infants. Hepat Mon 2009; 9(3):229-31. [ Google Scholar]
- Semnani S, Roshandel G, Abdolahi N, Besharat S, Keshtkar AA, Joshaghani H. Hepatitis B/C virus co-infection in Iran: a seroepidemiological study. Turk J Gastroenterol 2007; 18(1):20-1. [ Google Scholar]
- Younossi ZM, Otgonsuren M, Henry L, Venkatesan C, Mishra A, Erario M. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009. Hepatology 2015; 62(6):1723-30. doi: 10.1002/hep.28123 [Crossref] [ Google Scholar]
- Besharat S, Poustchi H, Mohamadkhani A, Roshandel G, Freedman ND, Merat S. Central obesity and advanced liver stiffness in hepatitis B: result from Golestan hepatitis B cohort study. Arch Iran Med 2015; 18(9):562-6. [ Google Scholar]
- Taheri N, Semnani S, Roshandel G, Namjoo M, Keshavarzian H, Chogan A. Aflatoxin contamination in wheat flour samples from Golestan province, northeast of Iran. Iran J Public Health 2012; 41(9):42-7. [ Google Scholar]